Author: Nikitha (Niki) Cherayil, MD
A. The Stem
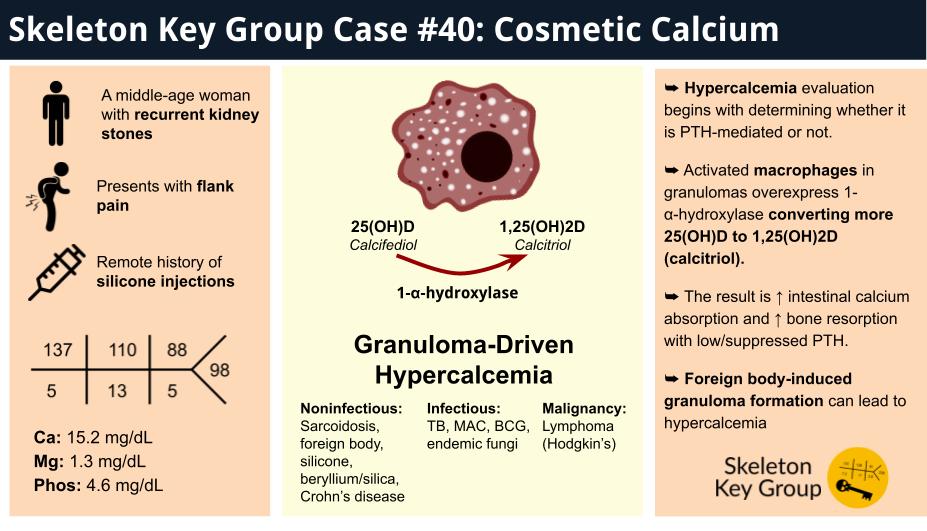
A middle-aged woman with chronic kidney disease stage 3 in the setting of hypertension and recurrent kidney stones presented to the emergency department with several days of right flank pain, dysuria, and hematuria. She had a history of similar episodes in the past requiring ureteral stenting and recognized the characteristic nature of the pain. Knowing that spontaneous resolution was unlikely given that the pain persisted, she presented to the hospital for evaluation of a possible recurrent kidney stone.
Imaging showed stent dislodgement into his bladder and obstructive nephrolithiasis, so she was taken urgently to the OR for right percutaneous nephrostomy tube placement.
Vital signs:
T 36.2 celsius (97.1°F)
HR 92 beats per minute
RR 19 per minute
BP 185/129 mm Hg
SpO2 98%
Physical exam:
Gen: awake, alert, in moderate distress
Heart: regular rate and rhythm, no murmurs
Lungs: clear to auscultation bilaterally
Abdomen: RUQ and R CVA tenderness, R percutaneous nephrostomy tube in place draining clear yellow urine
Extremities: moving all extremities spontaneously, no edema
Neurological: alert and oriented x3, labile mood
B. The Labs
ALP: 61 U/L
AST: 31 U/L
ALT: 18 U/L
Albumin: 4.4 g/dL
Total protein: 8.2 g/dL
Total bilirubin: 1.16 mg/dL
Due to her significant hypercalcemia, she was admitted to medicine for further workup and management.
C. The Workup
On further review of symptoms, the patient reported polydipsia, polyuria, constipation, and fatigue preceding the onset of acute right flank pain– all suggestive of hypercalcemia. A review of her previous hospital presentations revealed a pattern of progressively worsening hypercalcemia over several years.
General Approach to Hypercalcemia
Without further lab evaluation, a good history and medication reconciliation can identify many common causes of hypercalcemia. Usually longstanding hypercalcemia is indicative of primary hyperparathyroidism or a genetic etiology. Underlying comorbidities, like sarcoidosis or prolonged immobilization may also cause hypercalcemia. Given that primary hyperparathyroidism remains the most common cause of hypercalcemia, the diagnostic approach begins by determining whether the hypercalcemia is parathyroid hormone (PTH)-mediated or not. If hypercalcemia is found to be non-PTH-mediated, further evaluation should focus on potential causes such as increased intake, decreased kidney excretion, or increased bone resorption from an underlying pathologic process.
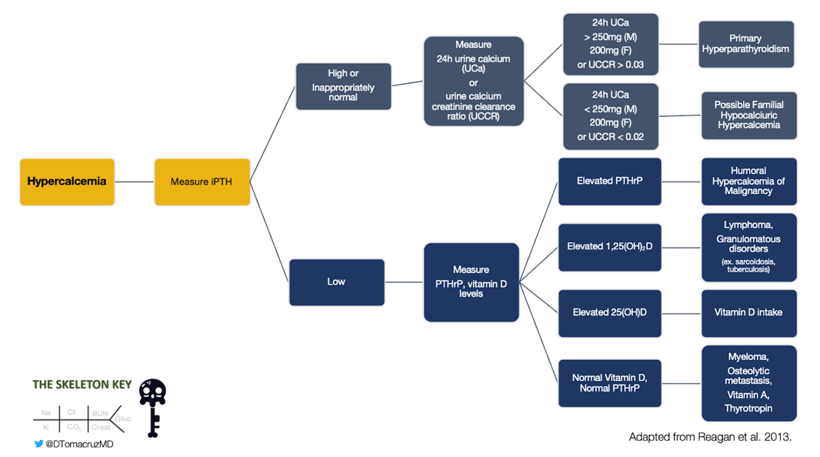
Figure 1: Diagnostic algorithm for hypercalcemia, adopted from Reagan, et al
Our Patient’s Evaluation
We started our evaluation with the most common etiology of hypercalcemia, hyperparathyroidism. The intact PTH (iPTH) was 34.1 pg/mL, which was inappropriately normal. We then proceeded to evaluate for other causes of hypercalcemia. Figure 1, which was first presented in Skeleton Key Group Case 10, shows one such algorithm for hypercalcemia workup.
Workup for hypercalcemia should start with a measurement of iPTH. This will tell us if it’s a PTH-mediated process or not.
If the iPTH is elevated or normal, the next branching point depends on a 24-hour urine calcium. If elevated, consider primary hyperparathyroidism where the parathyroids are producing more PTH which leads to calcium mobilization, and the kidneys, by seeing more calcium, are excreting more calcium. If the 24-hour urine calcium is decreased, then consider familial hypocalciuric hypercalcemia. This is a condition where the calcium-sensing receptors in the kidney are mutated and less sensitive to calcium, signaling the kidney to decrease excretion thus leading to hypercalcemia; patients present with mild hypercalcemia and normal to slightly elevated PTH.
If the iPTH is low, elevated for PTH-independent processes, such as:
-Malignancy (elevated PTHrP or osteolytic metastasis)
-Calcitriol-mediated process like lymphoma and granulomatous disorders (elevated 1,25(OH)2 vitamin D)
-Vitamin D toxicity (elevated 25(OH) vitamin D)
-Vitamin A toxicity (elevated vitamin A)
-Multiple myeloma (SPEP, UPEP)
-Thyroid disorders (abnormal TFTs)
The follow workup was obtained:
Given the significant elevation of our patient’s calcium, a lot of the workup was ordered at the same time and resulted at various points during her hospitalization. If we were to go through the algorithm for our patient though, her iPTH was inappropriately normal and her 24-hour urine calcium was elevated, which suggested primary hyperparathyroidism. However, given her underlying chronic kidney disease, the “normal” iPTH might reflect partial suppression from a chronically elevated baseline (we did not have a recent iPTH value to compare). That’s why we also considered other PTH-independent diagnoses, as well.
Going through the PTH-independent side of the algorithm
-PTHrP was negative ruling out PTHrP malignancy (Quick note: certain PTHrP assays may increase due to decrease in eGFR depending upon if C- or N- terminal is measured)
-25(OH) vitamin D was decreased ruling out vitamin D toxicity
-SPEP was negative ruling out multiple myeloma
-Vitamin A was normal ruling out vitamin A toxicity
-TFTs were close to normal, ruling out significant thyroid disorders
We also evaluated for sarcoidosis with an ACE activity level which was normal and rhabdomyolysis with a CK level which was negative. Imaging ruled out pituitary adenomas, obvious malignancies, and sarcoidosis as well. Her 1,25(OH)2 vitamin D (calcitriol) level was significantly elevated and 25(OH) vitamin D was decreased, which led us to believe that a calcitriol-mediated process was significantly driving the hypercalcemia. Calcitriol-mediated causes of hypercalcemia are summarized in Figure 2:
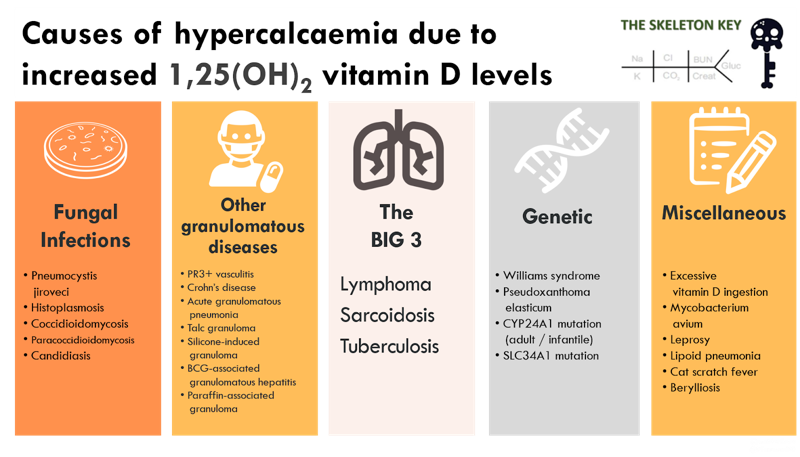
Figure 2: Causes of hypercalcemia associated with high 1,25(OH)2 vitamin D levels. Adapted from Tebben and Jacobs
Our workup thus far had ruled out many of the above diagnoses including fungal infections, tuberculosis, sarcoidosis, obvious malignancies, and excess vitamin D ingestion. The patient did not report a family history of hypercalcemia. We were leaning towards a more occult malignancy and were trying to get a PET scan, when we looked back through our imaging. Embedded in the CT abdomen/pelvis report was this finding: bilateral soft tissue changes in the bilateral upper thigh regions from foreign body insertion and nonspecific bilateral inguinal lymphadenopathy.
In further history, the patient endorsed receiving several silicone injections to the bilateral thighs regions for augmentation in the 1990s. Physical examination revealed induration and hyperpigmentation of the upper thigh areas, with cobblestone contouring and irregular dimpling.
D. The Diagnosis
This was a middle-aged woman who presented with persistent, symptomatic hypercalcemia manifesting primarily as recurrent nephrolithiasis. Laboratory workup suggested a calcitriol-mediated hypercalcemia. Clinical history, physical examination, and imaging findings were suggestive of silicone-induced granulomatous disease as the underlying cause.
A skin biopsy was done to confirm our diagnosis. The pathology report described empty spaces surrounded by sclerotic stroma consistent with a foreign substance injected within the deep dermis without evidence of granuloma formation. Since there were no other sources of the hypercalcemia, it was suspected that the biopsy missed the granulomatous areas, representing a sampling error.
Silicone is FDA-approved for breast implants but used off-label for other body contouring like gluteal, pectoral, calf, abdominal, and facial contouring. Hypercalcemia from granuloma formation has been reported as a chronic complication. Other chronic complications include tissue necrosis, and even issues related to silicone leakage and migration to nearby or distant tissues. In 2013, one case study found 28 cases reported in news articles and lawsuits documenting hypercalcemia caused by silicone injections with a geographic predominance in Florida (35.7%), Texas (14.3%), and California (10.7%). Since the use of silicone implants and cosmetic injections is increasing, it is important to be aware of this diagnosis in patients with hypercalcemia.
Why does silicone cause hypercalcemia? It causes granulomatous disease. Macrophages aggregate around foreign material when the immune system is unable to digest it. This accumulation of macrophages isolating the foreign material results in granuloma formation.
Macrophages produce interferon gamma, which stimulates the production of 1-alpha hydroxylase. This enzyme converts 25(OH) vitamin D to the active form 1,25(OH)2 vitamin D (calcitriol). Interferon-gamma also inhibits the enzyme 24-hydroxylase which degrades calcitriol. This results in PTH-independent calcitriol-mediated hypercalcemia as detailed in Figure 3.
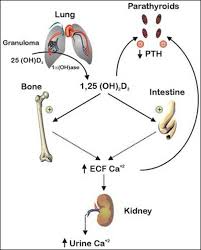
Figure 3: Mechanism of hypercalcemia in granulomatous diseases as illustrated by Goltzman
Understanding the pathophysiology of PTH-independent calcitriol-mediated hypercalcemia is important when learning about the possible treatments for this diagnosis.
E. Management
We’re aware of the short-term management of hypercalcemia, which includes IV fluids, diuretics, calcitonin, and bisphosphonates, which can also be used as temporizing measures when managing this specific diagnosis. Other treatments include steroids, which can reduce granuloma formation and suppress 1-alpha hydroxylase. Long-term use of steroids obviously has its disadvantages. The only curative option is surgical removal of the granuloma(s). As shown in Figure 4, the treatments used to manage the patient’s hypercalcemia, excluding IV fluids, are summarized. Surgery was consulted for excision, but it was not possible due to the extent of fibrosis.
Other options that have had or have been theorized to have some success in this granuloma-mediated hypercalcemic conditions are:
-Ketoconazole: inhibits 1-alpha-hydroxylase which is a CYP450 enzyme.
–Hydroxychloroquine: inhibits the activation of 1-alpha hydroxylase.
-TNF-alpha inhibitors: TNF-alpha is a cytokine that promotes granuloma formation and maintenance. It is also involved in osteoclast formation and activity
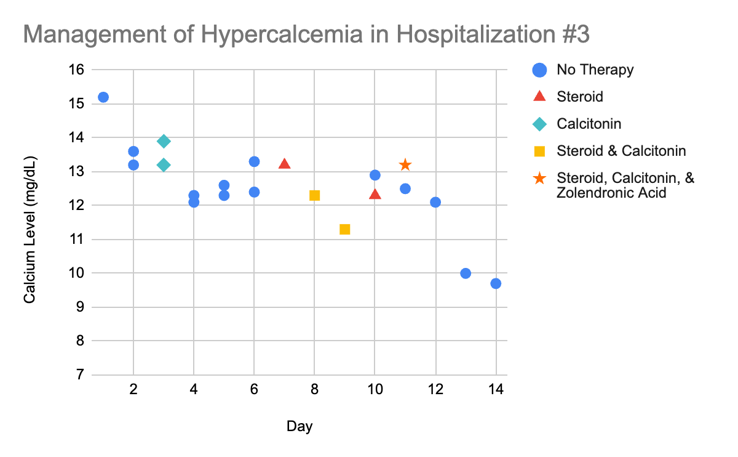
Figure 4: Management of Hypercalcemia during hospital stay
F. Take Home Points
- Hypercalcemia can cause kidney stones, constipation, nausea, fatigue, bone pain, psychiatric problems, and organ damage.
- Evaluation of hypercalcemia relies on understanding the most common etiologies, with primary hyperparathyroidism being by far, the most common cause. The first step is thus figuring out if the hypercalcemia is PTH-mediated or not.
- Activated macrophages in granulomas overexpress 1-α-hydroxylase converting more 25(OH)D to 1,25(OH)2D (calcitriol). The result is ↑ intestinal calcium absorption and ↑ bone resorption with low/suppressed PTH.
- Foreign body-induced granuloma formation resulting in hypercalcemia should only be suspected in a person with history of a retained foreign body when other more common etiologies have been ruled out.
- Surgical removal of granulomas is the only curative treatment of this condition. There are limited options if surgery is not an option, and more research needs to be done to explore medical management.
Editors: Jefferson L Triozzi, MD MSCI, Marc Lawrence Soco, MD, Chi Chu MD, Joel Topf, MD, Matthew A. Sparks, MD
Reviewed by: Srinath Yadlapalli, M.D.