A 50 yo male with non-ischemic cardiomyopathy with ejection fraction of 15% presented with worsening dyspnea and renal failure (Cr 3 mg/dl). He was started on inotropes and was evaluated for heart transplantation.
Nephrology was called since the treating physician thought this patient might benefit from a combined heart-kidney transplant. The presented argument on the first phone call was that by doing a combined transplant, we would decrease the need for a repeat surgery in the near future for a kidney transplant and possibly benefit of the lower rejection rate provided by combined organ transplantation.
In the past, renal failure was considered a contraindication for heart transplantation. Nowadays, we realize that many of these patients have a considerable improvement in renal function once the cardiac output is optimized with the new heart. However, can we predict which patients might require a combined kidney/heart transplant rather than a heart alone?
There are no randomized trials but a nice retrospective analysis from Columbia University suggest that neither the cause of heart failure nor the level of creatinine or proteinuria could reliably predict the renal pathologic diagnosis or the degree of tubular atrophy/interstitial fibrosis (TA/IF) of the native kidneys. The figure below shows the absence of correlation between eGFR at time of transplant and extent of TA/IF.
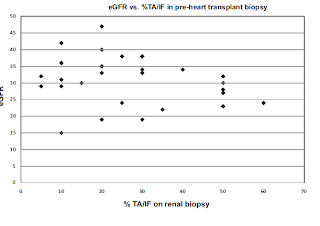
For example, two patients with ischemic cardiomyopathy, minimal proteinuria (100 mg/24 hr) and eGFR of 27.0 and 29.0 mL/min had TA/IF of 50% and 5%, respectively. Therefore, it seems prudent to perform a kidney biopsy on these patients. Certainly, other factors such as a prior high creatinine value and chronic changes on imaging could help, but based on the scarcity of organs, I believe the more information you have, the best decision you will make regarding organ allocation.
Overall, patients that undergo combined heart-kidney transplant (HKT) do well and the rejection rate is lower than after a single transplant. The immunological explanation might be related to an increase number of circulating donor leukocytes that could induce a microchimerism and promote tolerance. However, this simplistic theory is not accepted by all. Patients with significant renal scarring are probably the ones who might benefit the most of combined HKT. In addition, a retrospective analysis of UNOS data suggested that low-risk heart transplant recipients with eGFR less than 30 ml/min would benefit the most (as an example, a younger patient not on LV assist device and not dialysis-dependent). More info here.
The patient above had a kidney biopsy that showed ischemic nephropathy with less than 5% fibrosis. He was listed for a single heart transplant. His creatinine went down to 1 mg/dl one month after his heart transplant.




Thank you for your topic.
Can you provide more data on long term survival of these patients?
(I don t have access to the link you posted).
In context of shortage of organs, it is important that we need two organs to treat one and not two patients.
Anton Chrustowicz, JP2 Hospital in Cracow
anton_chrustowicz@yahoo.de
With liver cirrhosis, it is more challenging. I agree. However, there is well published data on the safety of performing transjugular kidney biopsy on those patients with minimal complications (below reference). Therefore, performing a kidney biopsy is probably appropriate in liver cirrhosis patients as well. For sure, if the patient has been on dialysis or has small highly echogenic kidneys on US, it is not worth biopsying. Individualizing the decision is always essential!
Sam R, Leehey DJ, Picken MM, et al. Transjugular renal biopsy in patients with liver disease. Am J Kidney Dis 2001; 37: 1144.
Another concern is when we do a kidney biopsy, are we doing it for the patient in question or for the "other" patient who would actually get the kidney in case the biopsy patient did not have enough fibrosis. This is more often a case in liver cirrhosis, when the bleeding risk is high and a kidney biopsy is attempted to assess for the need for combined LKT. The question asked by one of the family members of the patient who dies from extensive hhage from a kidney biopsy is "why was the biopsy done?" There is no strong evidence to support it.