 |
| This image was from Original Nate Hellman post in 2010 |
It’s Monday, I turn my pager on at 6:00am, and at 6:03am and again at 6:05am my pager promptly goes off. I recognize both of the numbers, it’s the emergency department, and I answer:
“Hi, this is the Nephrology fellow returning a page”
“Hey, I’m calling from the emergency department, we have 6 patients that qualify for emergent dialysis and 4 more just walked in… I’ll call you back if they meet criteria…”
As the ESRD fellow at Ben Taub Hospital in Houston Texas, I receive these pages multiple times on a daily basis. With attending supervision, my job is to assess the number of patients in the hospital that require dialysis and then count how many nurses/machines are available each shift to accommodate the remaining emergent dialysis patients.
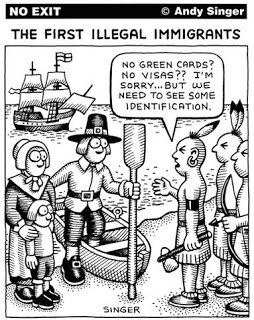
Emergent dialysis patients are individuals who do not have a assigned dialysis unit and present to the hospital with symptoms necessitating an acute dialysis treatment. What does one mean by ‘patients who do not have a dialysis center home’? In our institution, over 95% of them are undocumented immigrants. While US citizens are covered by Medicare/Medicaid or other secondary payers, undocumented immigrants are ineligible for these resources. Under usual circumstances and in accordance with published recommendations, patients with ESRD should have dialysis 3 times a week in an outpatient dialysis unit. But for emergent dialysis patients, in many states including Texas – they present to the ED for therapy and are only dialyzed after meeting criteria for emergent dialysis.
| From Raghavan Semin Dialysis 2012 |
Criteria (see figure above) for emergent dialysis vary from each hospital but usually include: hyperkalemia, acidosis, volume overload, hypoxia and uremic symptoms. Patients who do not meet criteria are often turned away if no dialysis spots are available. Despite knowing they really do need dialysis that day, they have to wait till they become sick enough to qualify. To be emergent enough. We’ve had some patients/family members who come to the hospital dialysis unit and get angry at staff when they didn’t meet criteria. Other patients, put themselves in harms way to meet criteria. I have even heard of patients taking potassium supplement in an effort in induce hyperkalemia and thus allow for dialysis. I very risking proposition that has in the past led to arrhythmia and near fatal arrest.
The quality of life for these patients is poor, both physical and mental health were lower compared to patients on scheduled dialysis. In addition to this, compared to standard dialysis, emergency only dialysis has a higher death rate and is also nearly 4-fold more costly due to the greater number of ED visits and death: Providers are also at a disadvantage when caring for these patients. With limited spots, as fellows we are constantly trying to figure out which patients and how many patients can we accommodate daily. Furthermore, obtaining vascular access, adequate predialysis/dialysis care and affordable medications are other factors which makes care for these patients difficult.
We have known about this for a while: see Nate Hellman’s post on this from 8 years ago. There has been increasing attention focused on it in recent years, especially with the article in JAMA IM on patient experiences (see the #NephJC discussion). Some states including California, New York, Illinois and Washington do offer scheduled dialysis by using non-federal funds and other states even allow kidney transplantation,but very limited options are available in Texas. Recently, purchasing off-ACA exchange commercial health insurance plans have been tried, however they can be expensive for undocumented individuals considering 40% have annual incomes below the Federal Poverty Level.
Without citizenship, our undocumented patients with ESRD suffer with poor quality of life, worsened prognosis, increased cost and limited support. Clinicians must continue to lobby for a policy to create a better system for patients and those taking care of them.
Natasha Dave
Nephrology Fellow
Baylor Houston
NSMC Intern Class of 2018


