Based on previous studies, the kidney is the most common site of extra hematopoietic involvement in hematologic malignancies, up to 90% in certain series. As with any other kidney disease, the approach to acute kidney injury (AKI) should try and distinguish between pre-renal, intrarenal, and post-renal causes. Here, we will focus on intra-renal causes of AKI that develop due to leukemias and lymphomas. Intra-renal AKI can be divided by the site of injury: the vasculature, glomeruli, tubules, and interstitium.
Renovascular Injury:
Renovascular disorders associated with malignancy have multiple mechanisms. Lymphomas have been associated with the production of antiphospholipid (APL) antibodies, with consequent thrombosis of the renal artery and/or renal vein. Of note, APL antibodies may become negative with adequate treatment of the underlying malignancy. Malignancies with high white blood cell counts such as myeloid leukemias may rarely present with leukocyte thrombi and fibrin clots in the kidney vasculature. Hemolytic uremic syndrome (HUS) is a condition mostly seen in the pediatric population after initiation of chemotherapeutic agents. Simultaneous presentation of HUS with acute lymphoblastic leukemia before commencement of treatment has been reported.
Glomerular Injury:
The association of glomerular diseases with malignancy is well-recognized, with certain glomerular lesions more specific to particular hematologic malignancies. Hodgkin’s lymphomas may cause multiple glomerular pathologies (most commonly minimal change disease, MCD) which can precede the diagnosis in a third of cases. Less often, focal segemental glomerulosclerosis (FSGS), pauci-immune crescentic glomerulonephritis (GN), and anti-glomerular basement membrane disease can be seen.
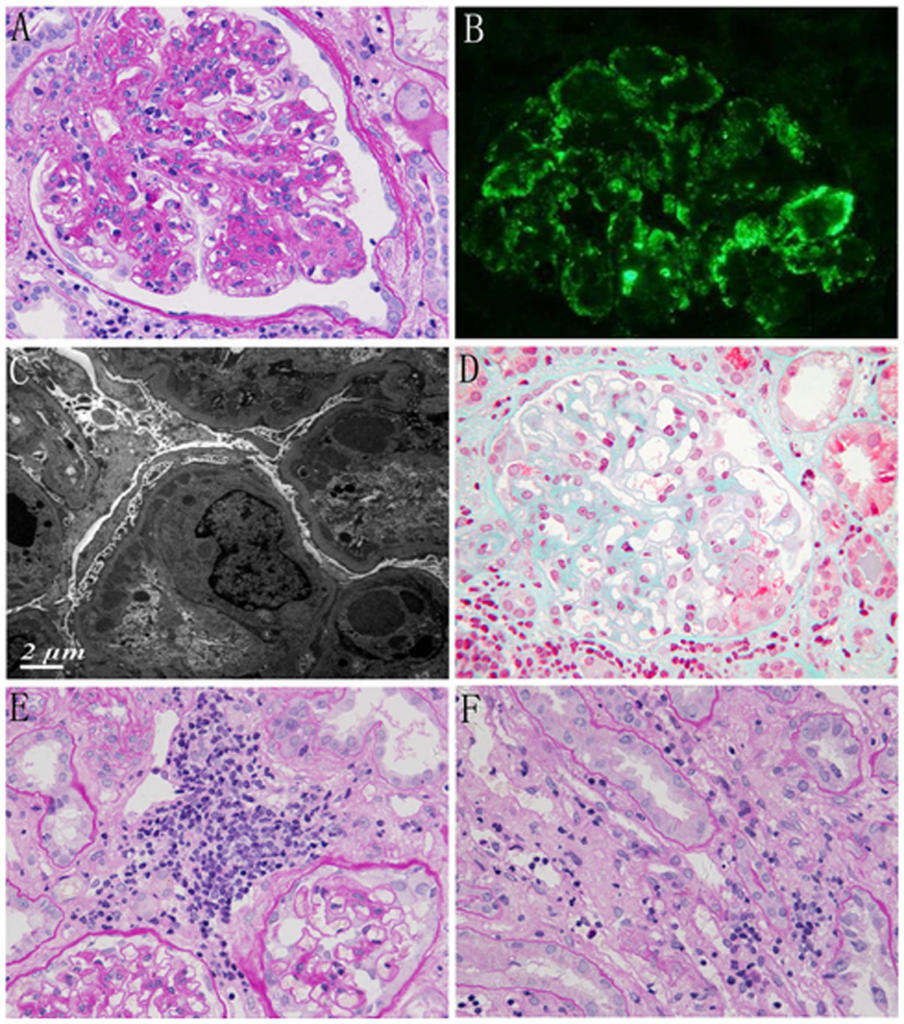
Non-Hodgkin’s lymphomas, through the production of cytokines and subsequent immune complex deposition, predominantly causes proliferative lesions such as membranoproliferative GN (MPGN) (Fig 1). Acute lymphoblastic and myeloid leukemia may uncommonly cause MPGN, FSGS, and MCD, though they are more commonly known for causing lysozyme-induced nephropathy.
Tubular Injury:
Tubular disorders, in particular acute tubular necrosis (ATN), are the most common causes of intrinsic AKI, with sepsis and medications being the typical precipitating events. Described in the 1960s, lysozyme-induced ATN is a less common cause of AKI. Lysozymes are a cationic proteins excreted by monocytes and macrophages which are freely filtered by the glomerulus and reabsorbed in the proximal tubule. In certain hematologic malignancies, especially monocytic and monomyelocytic leukemia, high concentrations of lysozymes can cause ATN as well as kaliuresis with subsequent hypokalemia and proteinuria. Measurement of serum and urine electrophoresis exhibiting high gamma globulin levels may provide the first clue to diagnosis. Immunofixation electrophoresis should be also performed to look for evidence of monoclonal gammopathies.
Interstitial Injury:
Kidney infiltration by hematologic malignancies is common (Fig 2), however AKI secondary to infiltration is rare. Nevertheless, when this is bilateral and predominantly in the interstitium, increased pressure may lead to increased tubular pressures, tubular obstruction and compression of peritubular capillaries leading to ATN. In most cases, kidney function should improve with chemotherapy or radiotherapy.
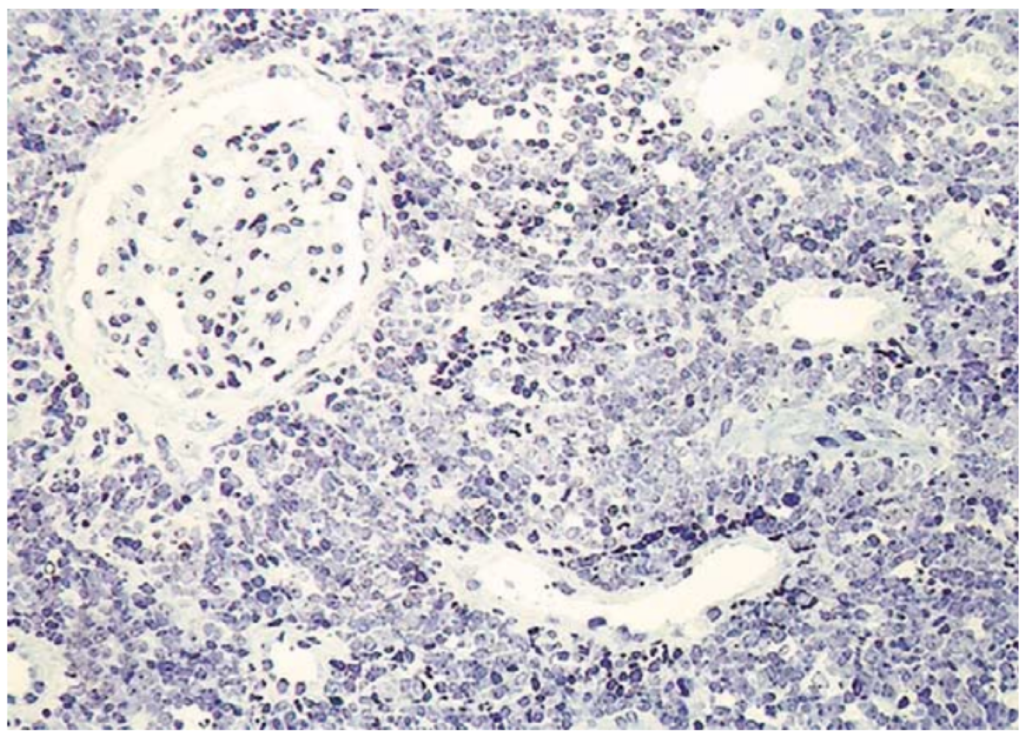
In summary, hematologic malignancies can cause kidney damage through multiple mechanisms and affect various compartments of the kidney. The approach should be the same as in other forms of AKI. Imaging studies may demonstrate enlargement of both kidneys in cases of malignant infiltration and kidney biopsy may help confirm the etiology of kidney injury.
Post by: Mario Funes, MD
NSMC Intern, 2019


