Introduction:
Welcome to the third piece in the Home Hemodialysis series. After going through the history of home hemodialysis in the United States, and reviewing the literature evaluating the modality, we will now dive into how to prescribe home hemodialysis.
But before we do, there are a few general themes to know:
- While the traditional machines and prescriptions used in in-center home hemodialysis can be applied at home, (and this indeed was how home hemodialysis was performed prior to approval of the NxStage system by the FDA in 2005), urea kinetics, and therefore the prescription, are similar to that seen in in-center hemodialysis.
- With now over 85% of patients in the United States that are on home hemodialysis using the low dialysate volume approach (on the NxStage system), and almost all new patients initiated on home hemodialysis being initiated with this treatment strategy, we are, in the rest of this piece, going to be learning to write a prescription for the low volume dialysate approach.
- The major advantage of the low dialysate volume approach, as is intuitive by the description, is the utilization of lower volumes of dialysate to achieve similar clearances – while the weekly dialysate volume used in traditional hemodialysis is around 270 to 600 L per week, at flow rates of 600-800 ml per minute, the low dialysate volume approach utilizes 90 to 200 L per week, at flow rates of 100-200 ml per minute.
- A disclaimer about the utilization of Kt/V(urea) to determine dialysis adequacy must be part of all discussions regarding dialysis prescriptions. However, though imperfect, it remains to-date the most widely used measure, and has been used to build home hemodialysis prescriptions as well. One must remember to assess the patient on multiple parameters – including symptoms of uremia, volume status, electrolytes, nutritional status, and not just rely on Kt/V to make changes to any dialysis prescription.
Now let us really dive in.
The concept of clearance and urea kinetics in the low dialysate volume approach:
The low dialysate volume approach is based on the principle of the dialysate fluid being nearly completely saturated with urea, by lowering the dialysate flow in comparison to the blood flow – the slower dialysate flows as it opposes blood, the more time for mass transfer and saturation with urea.
The concept of the dialysate fluid being maximally saturated with urea is similar to peritoneal dialysis – and this is very helpful to remember, as calculating the urea clearance, and Kt/V for the low dialysate volume approach is similar to peritoneal dialysis.
For example,
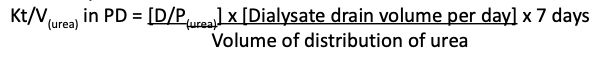
Similarly,
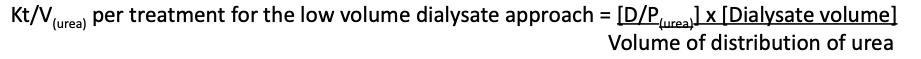
We know that D/P(urea), or the saturation of dialysate fluid with urea, is determined by the dialysate flow relative to the blood flow. This brings us to an important component of the prescription in the low dialysate volume approach – the flow fraction (FF). This is the ratio of dialysate flow (Qd) to the blood flow (Qb), or Qd/Qb – the higher the flow fraction, lower the dialysate urea saturation. With standardization of the flow fraction comes standardization of dialysate saturation – for each treatment, this ratio is fixed, which allows for the dialysate flow rate to be adjusted automatically by the machine in response to any changes in blood flow that may occur, without the need for patient intervention, to maintain a desired saturation of urea. This assures that even in the setting of inability to maintain the targeted blood flow rate, e.g. during access stenosis, that the patient receives the same amount of clearance intended, but at the cost of time.
As it can be seen from figure 1, at a FF of about 40%, the dialysate is about 90% saturated with urea.
Let us recap one last concept, with the help of another key figure, before putting it all together as a home hemodialysis prescription.
The target single pool Kt/V for 3 times a week in-center hemodialysis is about 1.2 to 1.4. Three weekly treatments with a single pool kt/v would provide a weekly standard kt/v of about 2.0. It is important to remember that the relationship between single pool and standard kt/v is not linear and the weekly clearance is not merely the sum of the clearance of each treatment. In home hemodialysis, as the number of sessions per week are higher, the target per session Kt/V is lower, around 0.5 to 0.6, depending on the number of sessions per week, to achieve a weekly standard Kt/V of 2 to 2.2
Now, with the above information, let us calculate the urea kinetics for an 80 kg female (height 160 cm, age 55 years), who will perform home hemodialysis 5 times a week using the low dialysate approach
Her target per session Kt/V is 0.6
Her volume of distribution of urea is about 34L (the most common equation to calculate the total body water from weight is the Watson equation – access at http://www.medcalc.com/tbw.html)
Now we know that,

Thus,
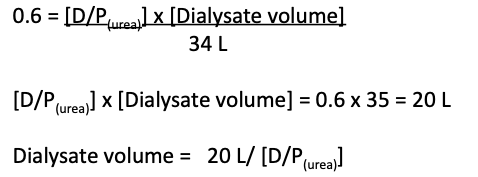
Now if we assume 100% saturation of dialysate fluid with urea, the D/P(urea) = 1, and we would need 20L of dialysate to achieve a per session Kt/V of 0.6. In this scenario, the filtration fraction would have to be <10%.
A more typical approach is to use filtration fraction of about 40-50%, which achieves dialysate saturation of about 90%. Therefore, modifying our above prescription accordingly,
Dialysate volume = 20/ 0.9 = 22L
The prescription:
Now that we understand the urea kinetics of the low volume dialysate approach, writing a prescription is the next intuitive step.
Any hemodialysis prescription requires the following parameters
- Blood flow (Qb)
- Dialysate flow (Qd)
- Time on dialysis
- Dialysate volume
- We will be adding filtration fraction (FF) as an additional parameter for home hemodialysis.
In in-center hemodialysis, we define Qb, Qd and time on dialysis, and the dialysate volume, and FF are dependent on these variables, while in home hemodialysis, we define FF, dialysate volume, and Qb, and time on dialysis, and Qd are dependent on them.
For our 80 kg female, we determined we needed 22L of dialysate fluid, if a filtration fraction of about 40% was used. Thus, we know that
Dialysate volume = 22L
FF = 0.4
Qb is typically similar to that of traditional hemodialysis – let us assume a great AV access, with blood flow of 400 ml per minute.
Thus Qd = 0.4 x 400 = 160 ml per minute.
The time on treatment is not usually prescribed, but is determined by the dialysate volume required, and the dialysate flow, which is this case, is 22000/160, about 140 minutes, or 2 hours 20 minutes.
However, as I was recently reminded, the more patient-centric parameter is time on dialysis. This would also be an important consideration if the patient requires a fixed amount of time on dialysis to achieve goal volume status. The prescription can therefore be manipulated to provide a fixed, desired time on dialysis.
Again, for our 80 kg female, we determined we needed 22L of dialysate fluid, if a filtration fraction of about 40% was used. Thus, we know that
Dialysate volume = 22L
FF = 0.4
Let us assume this patient requires 2.5 hours on dialysis each day to achieve net ultrafiltration of 2L
Thus, the 22L of dialysate will be used over 2.5 hours (150 minutes) at the rate of 22000/150 or approximately 148 ml per minute of dialysate flow rate.
To maintain a filtration fraction of 0.4, the blood flow rate will then have to set based on the calculated dialysate flow rate – 148/0.4, or approximately 370 ml per minute.
Knowing the basics of how a prescription though tedious, helps with then understanding why a particular prescription isn’t working for a patient, and thus with trouble-shooting.
Final Tips:
A few final tips to remember
- Remember that the dialysis adequacy in home hemodialysis is calculated similarly to peritoneal dialysis – so:
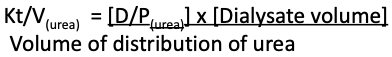
- Remember that with a goal Kt/V per session of about 0.55 to 0.6 for 5 treatments a week, and 0.45 to 0.5 for 6 treatments a week, an initial dialysate volume required per session can be estimated
- Remember the filtration fraction – the ratio of Qd/Qb, which is fixed.
- Remember that roughly, a filtration fraction of 0.4 results in a 90% dialysate saturation with urea (or D/P(urea) = 0.9 with a filtration fraction of 0.4)
- Remember that with a dialysate volume, and filtration fraction, the rest of the parameters of a home hemodialysis prescription – blood flow rate, dialysate flow rate, and time – can be calculated
- And finally, remember to not to be too focused on the Kt/V. Think about the patient!
Want to know more? Here are some additional resources
AJKD Home Dialysis Curriculum https://www.ncbi.nlm.nih.gov/pubmed/19748715
Managing Kidney Failure on Home Hemodialysis
Next up in the series – have you seen the water treatment room in your dialysis unit? Now think about how this reaches patients on home hemodialysis!
Madhuri Ramakrishnan, MD
Nephrology Fellow, Washington University School of Medicine in St. Louis


