Introduction
Light chain cast nephropathy (LCCN), not to be confused with light chain deposition disease (LCDD), is also known as myeloma cast nephropathy or myeloma kidney; and is one of the many renal complications of multiple myeloma. Patients affected generally have an established diagnosis of multiple myeloma and as can be expected, are typically middle aged to older adults. It is the most common histopathological finding in patients with multiple myeloma and renal dysfunction with a prevalence of 30-50%. Rarely LCCN can be the initial presentation of a subclinical or smoldering myelomatous process, and therefore this diagnosis must be high on the differential for older patients who present with acute kidney injury.
Clinical presentation
Renal dysfunction from cast nephropathy can either be acute or progressive over time and can develop at any point during the course of the disease. There can be superimposed renal disorders such as tubular dysfunction (due to direct toxicity from light chains), amyloidosis, various types of immune complex mediated disease, alternative complement pathway dysregulation etc. Proteinuria is usually nephrotic range though urinalysis is not reflective of this as the proteins consist mainly of light chains and not albumin.
How do the casts form and how do they induce injury?
Free light chains (FLC) circulating predominantly as kappa and lambda are freely filtered by the kidneys and initially reabsorbed by the proximal tubular cells (PTC) where they cause injury and PTC dysfunction. The now dysfunctional proximal tubular cells are overwhelmed by the filtered load of free light chains and allow their passage to the distal tubules where they aggregate with Tamm-Horsfall proteins (THP) secreted by the thick ascending limb (TAL) of the loop of Henle. The light chain-THP interaction leads to cast formation which in turn causes tubular obstruction as well as tubular basement membrane rupture and subsequent renal dysfunction. The presence of the casts in the tubules also elicits an inflammatory reaction and if persistent, to the rapid development of interstitial fibrosis.
What determines cast formation and renal injury?
It has been shown that inhibition of the light chain/Tamm-Horsfall protein interaction prevents cast formation. The successful interaction of the light chains and Tamm-Horsfall proteins is apparently modulated by the physiochemical features of the light chains. Specifically, the variability of the CDR3 domain of the light chains leads to varying affinity to THPs such that not all light chains successfully form casts. Volume depletion, furosemide, urinary acidification and favorable ionic environments such as high urine concentrations of sodium and calcium all promote cast formation.
Light microscopy
It is important to know the classic histologic features of light chain cast nephropathy, as in some cases the presence of LCCN may be the initial presentation of an underlying subclinical myelomatous process.
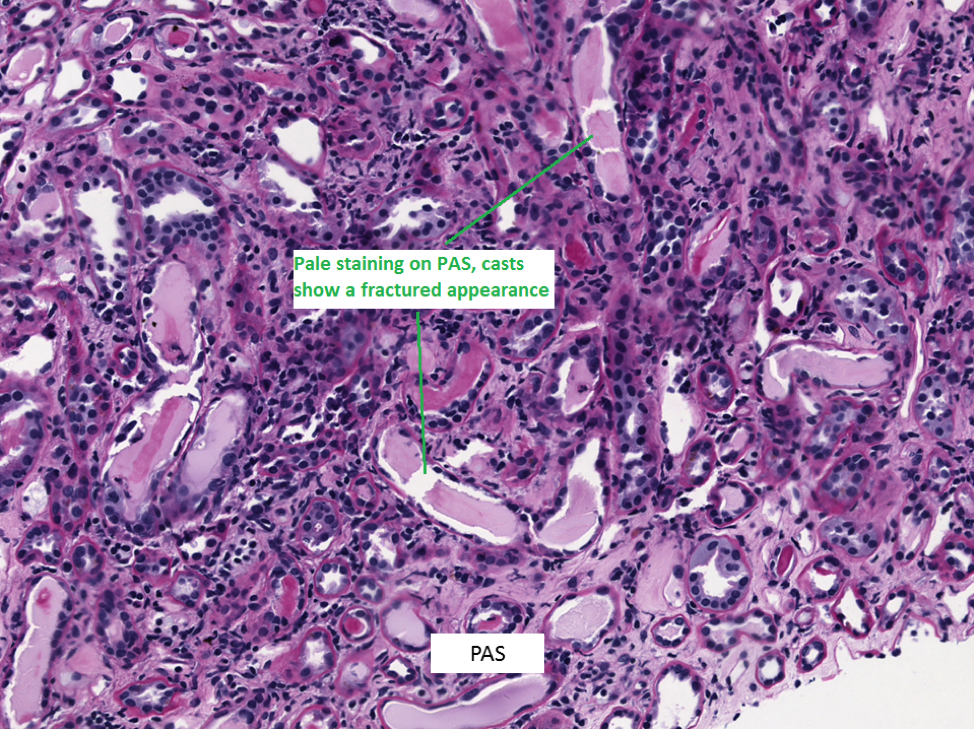
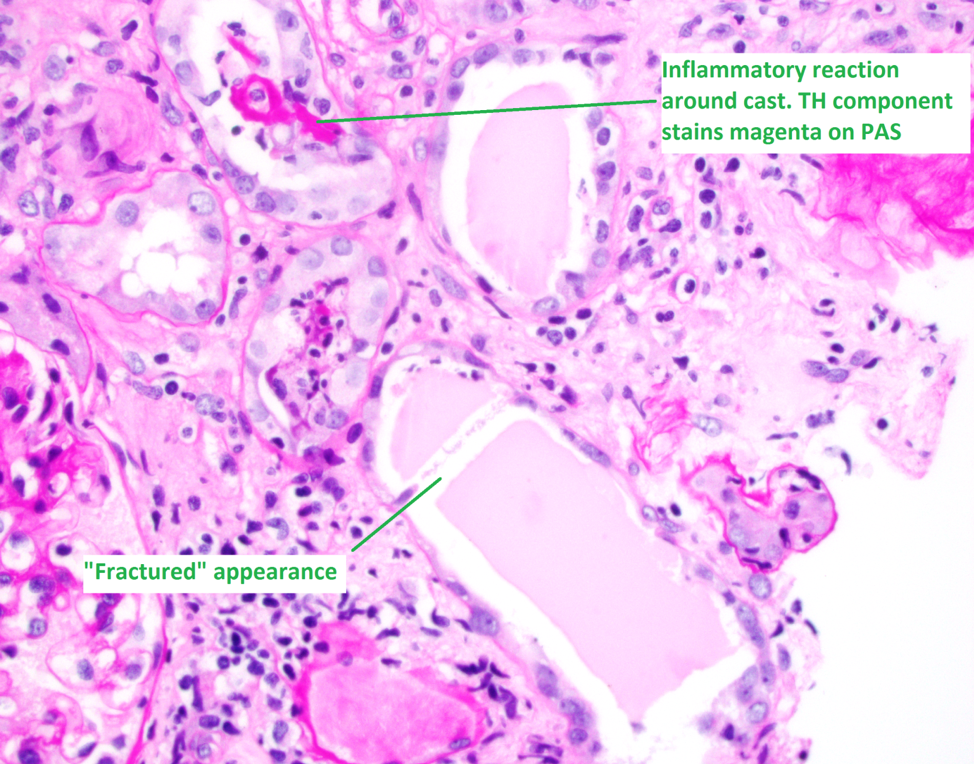
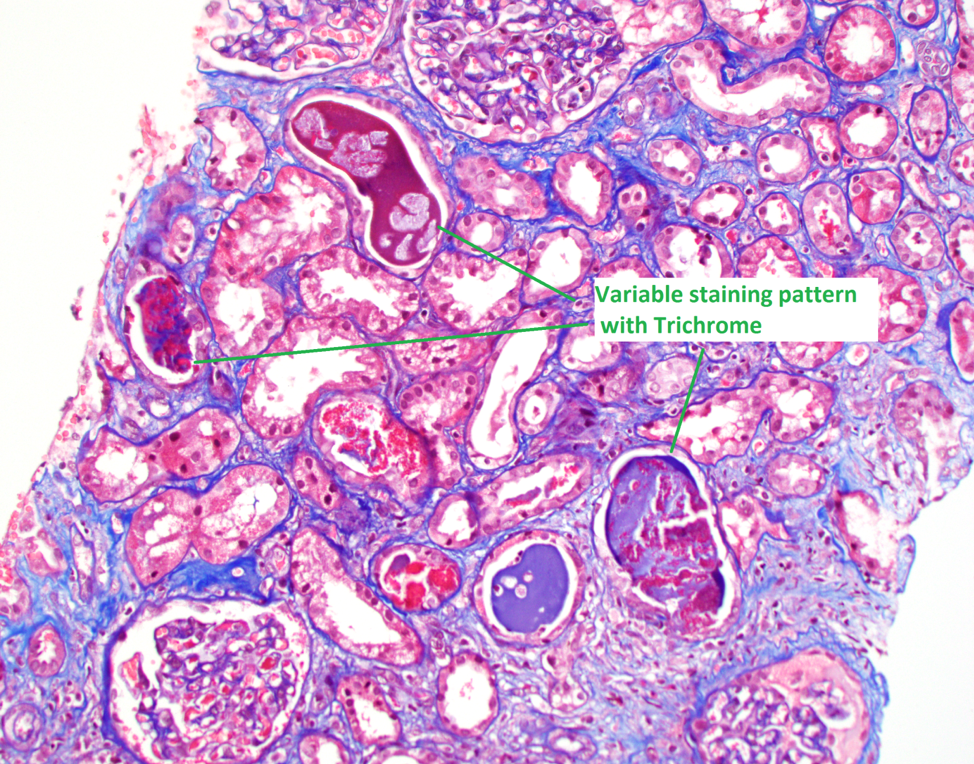
1. Light chain casts have an eosinophilic appearance on H&E stain, with a pale/light pink appearance on PAS. In contrast to this TH protein casts and hyaline casts are positive on PAS, staining a bright magenta color.
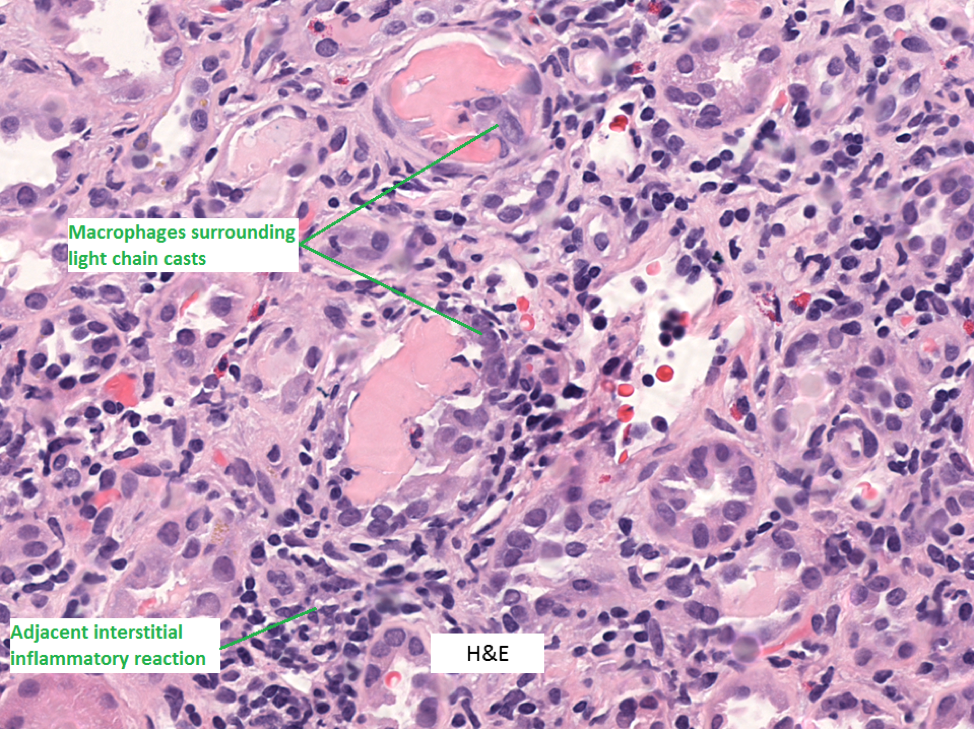
2. LC casts usually have a “fractured” appearance on light microscopy. This is a histotechnology sectioning artifact that occurs due to the hard/rigid nature of the casts, which is not seen in TH or hyaline casts which are softer.
3. LC casts elicit an inflammatory response in the adjacent interstitium. The casts themselves are often surrounded by intraluminal macrophages and sometimes multinucleated giant cells.
Immunofluorescence
Monoclonal restricted light chain staining (kappa or lambda) of the atypical casts is the characteristic finding. IF staining after antigen retrieval is usually not needed to confirm monoclonality of the casts, but it may help to reveal the presence of light chain proximal tubulopathy (LCPT) which can be concurrently present.
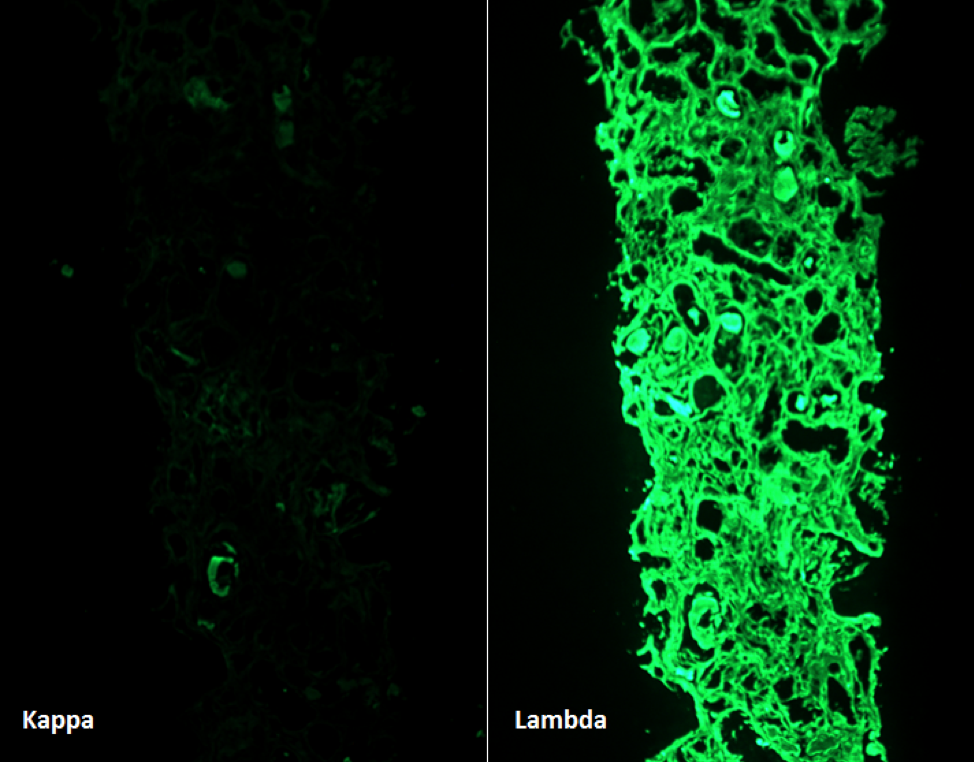
It should be noted that the presence of a few monoclonal staining casts, without classic histologic features, is not enough for a diagnosis of LCCN. Classic histologic features, evidence of an active inflammatory response to the casts, and monoclonal staining should all be present in order to make this diagnosis.
Treatment
Initial management
The focus of treatment is rapid, substantial and sustained reduction in the serum FLC burden as this has been shown to promote renal recovery. In addition, factors that facilitate the precipitation of casts should be avoided or corrected if already present. Intravascular volume expansion to maintain high urine flow is important and high fluid intake (3L/day) should be maintained subsequently. Bortezomib, a reversible proteasome inhibitor, in combination with dexamethasone, for the prompt reduction of serum free light chains, is of benefit in patients with renal dysfunction as its clearance is not dependent on renal function. Immunomodulatory medications such as thalidomide, pomalidomide and lenalidomide have also been shown to be of benefit.
Additional treatment
Studies on the benefits of extracorporeal therapies have been controversial at best with some studies showing significant reduction in the burden of serum FLCs with three or more plasmapheresis sessions and others demonstrating no benefit. Studies investigating the benefit of high cut off hemodialysis (HCO-HD) have been discordant as well with some suggesting early and sustained decrease in the sFLC burden and independence from dialysis and others showing no advantage when compared to conventional dialysis. A cohort study in 2017 investigating the effectiveness of IHD with adsorptive PMMA membrane in myeloma cast nephropathy suggested high rates of renal recovery and survival and may merit further investigation.
Chidinma Enyinna, MD
Fellow, UCSF Nephrology
For the next few months, the focus of the biopsy series will be on various features of Myeloma kidney- stay tuned.


