Welcome to the fourth case of the Skeleton Key Group, a team of twenty odd nephrology fellows who work together to build a monthly education package for Renal Fellow Network. The cases are actual cases (without patient identifying information) that intrigued the treating fellow.
Case 4: Written by Kartik Kalra.
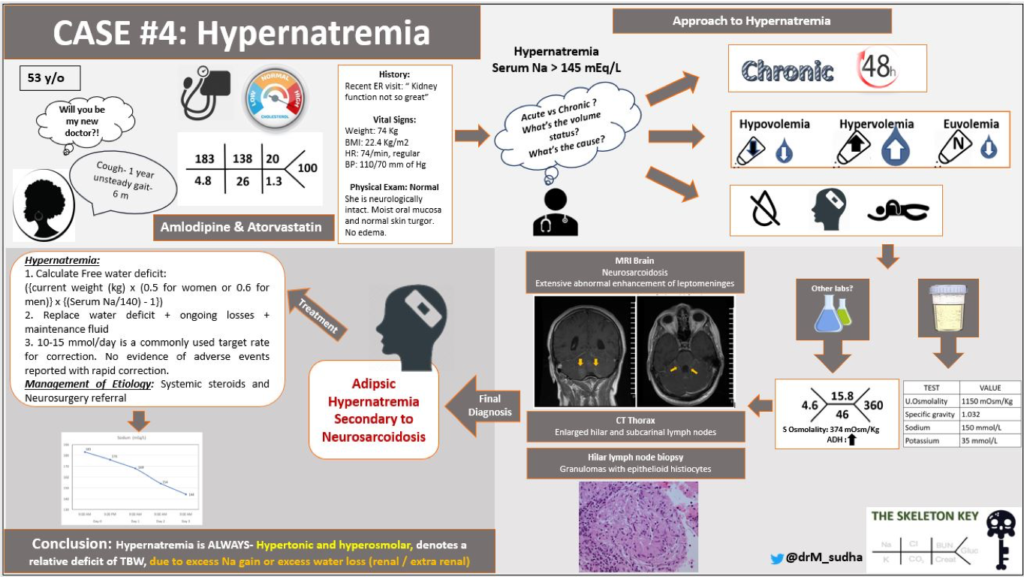
A. The Stem
A 53 year old female with a past medical history of hypertension and hyperlipidemia comes to your office to establish care. She has not seen a doctor in the last 6-8 months. She had one trip to an urgent care center eight months ago for a persistent, non-productive cough. At that time, she was told to follow up with a kidney doctor as her kidney function was “not great.” Additionally, she has a six month history of an unsteady gait. She denies any falls but feels dizzy at times. No one in her family has kidney disease. She does not smoke or consume alcohol.
Vital signs: Weight: 74 kg, BMI – 22.4 kg/m2, blood pressure: 110/70 mm Hg, heart rate: 74/min, regular
B. The Labs
Calcium 9.9 mg/dL, albumin 4.6 mg/dL
The patient was told to go to the emergency department immediately. In the hospital, she repeatedly denied any thirst. Her oral intake has been around 16 ounces of water a day. She does not have a history of weight loss, abdominal pain, constipation, diarrhea, or polyuria.
On exam, she is neurologically intact. Her oral mucosa is moist. She does not have any edema, excessive axillary sweat, and her skin turgor is normal.
Current medications: amlodipine 10 mg, atorvastatin 20 mg
C. Differential Diagnosis: Hypernatremia
Hypernatremia is defined as a serum sodium greater than 145 mEq/L. Hypernatremia always implies plasma hypertonicity. Thirst is a defense mechanism against hypernatremia. So, unless water intake is compromised (i.e decrease thirst response), hypernatremia will not develop.
The 3 means by which a patient does not drink water in response to an increase in the serum sodium:
- Water is inaccessible: e.g. lost in the desert
- Altered mental status: this is commonly seen in the intensive care unit, water is available and thirst mechanism is preserved but the patient is not awake or aware to drink or ask for water
- Altered thirst mechanism: in this situation, water is available and the patient is awake, but the patient does not feel thirsty because of problems with generating the neurologic sensation of thirst
D. More Data
Additional serum and urine studies:
Since the patient had an elevated serum sodium without thirst , this was a clear failure of the thirst mechanism to protect the patient from hypernatremia. This points to a central nervous system problem. The patient has appropriately concentrated urine, ruling out inappropriate kidney water losses (i.e. diabetes insipidus) as a cause.
Imaging was done to determine if there was an anatomic etiology for impaired thirst mechanism. Magnetic resonance imaging (MRI) of the brain showed extensive abnormal enhancement of leptomeninges (arrows):
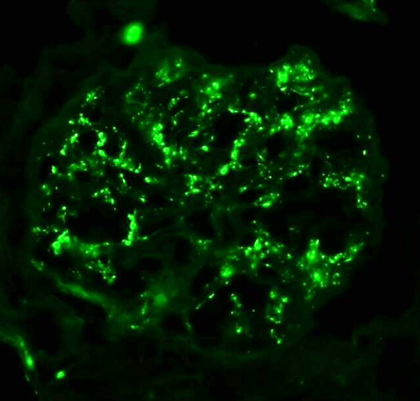
Due to her history of cough, a chest x-ray and computed tomography (CT) of the chest revealed enlarged paratracheal, subcarinal and hilar lymph nodes. The patient underwent hilar lymph node biopsy (below) which revealed epithelioid histiocytes and granulomas
E. Final Diagnosis & Management
Adipsic Hypernatremia Secondary to Neurosarcoidosis
Adipsia comes from the Greek “a,” which refers to “without,” and “dipsia” which refers to “thirst.” Overall adipsic hypernatremia is rare. This is because vasopressin release is stimulated when osmolarity rises above 280-290 mOsm/kg H2O, and thirst is triggered when the osmolality rises above 295 mOsm/kg H2O. Typically the condition results from structural abnormalities within the anterior hypothalamus or pituitary stalk, however there have been cases of possible autoimmunity, and other generalized neurologic conditions such as pseudotumor cerebri, subarachnoid hemorrhages, and meningoencephalitis.
Management
- The patient’s free water loss was calculated:
- ({current weight (kg) x (0.5 for women or 0.6 for men)} x {(Serum Na/140) – 1}) + Account for insensible losses
- [74 x 0.5 x (183/140–1)] which is approximately 11 liter
- Adding obligatory water loss via stool and skin (approx. 40 mL/h or 1 liter/ day)
- Adding urine free water loss was not performed in our patient, but to calculate urine free water losses use the electrolyte-free clearance equation
- Urine volume x (1- (Urine Na + Urine K) / serum Na)
- Total free water replacement required approximately 12 liter.
- 10-15 mmol/day is a commonly used target rate for correction of hypernatremia, but recent data suggest no evidence that more rapid correction was associated with greater risk of mortality, cerebral edema, or adverse events
- She was instructed to drink 500 mL of water every 3 to 4 hours regardless of thirst, and her sodium normalized over days.
How did the patient do?
- A follow-up sodium, a week after discharge, was 142 mEq/L
- Neurosurgery referral was obtained and patient was started on prednisone for her sarcoidosis
F. Let’s Talk About Hypernatremia
There are 3 different scenarios that may explain hypernatremia development:
Scenario 1. Sodium Excess
This usually occurs as a result of hypertonic fluid administration or excessive salt intake. Common fluid involved in this problem include NaHCO3 (8.4%, 100 meq in 100 ml). A case of this also was seen following an intentional soy sauce overdose.
Key feature: High urine osmolality. This can be seen after a successful resuscitation from a cardiac arrest after the patient receives multiple rounds of IV bicarbonate.
Volume Status: Hypervolemia. Gain of total body sodium as hypertonic fluid is responsible for this feature.
Scenario 2. Normal Water Loss
This is the result of normal water losses from urine, stool, and skin that go unreplaced because of inability to drink water causing a free water deficit.
Key features: High urine osmolality (Urine Osmolality ≥ 800 mOsm/kg): this is caused by the release of ADH in response to plasma hypertonicity. ADH acts on the kidneys to retain water and concentrate urine.
Volume status: Euvolemia. There is no gain or loss of total body sodium so the extracellular fluid (ECF) volume remains close to normal.
Scenario 3. Abnormal Water Loss
Excessive water loss can be either renal or extra-renal.
(A) Extra-renal water loss: Excess loss of hypotonic fluid from either gastrointestinal or skin sources.
Key features: High urine osmolality (UOsm ≥ 800 mOsm/kg): this is caused by the release of ADH in response to plasma hypertonicity. ADH acts on the kidneys to retain water and concentrate urine.
Volume Status: Hypovolemia.
(B) Abnormal Renal Water Loss (Scenario 2): This is caused by a lack of ADH activity in the kidneys to that the kidneys produce a large volume of hypotonic fluid. Seen in patients with diabetes insipidus (DI). Patients present with polyuria.
Key features: Low urine osmolality, usually less than 150 mOsm/kg . This is justified by low levels of ADH in the circulation acting on the kidneys, or alternatively, inability of the kidneys to respond to ADH ultimately causing a defect in urine concentration.
Euvolemia: Neither gain or loss of total body sodium is responsible for this feature.
In the acute setting, hypernatremia is treated by replacing the missing water, either orally (preferred) or by intravenous free water infusion (with dextrose) if the patient is unable to drink and does not have an enteral tube. For volume depleted patients, first correct volume deficit with normal saline until signs of volume depletion are no longer present.
Regardless if acute or chronic, Joel Topf, MD suggests a “Yesterday, Today, Tomorrow” framework for calculating the correction needs. This approach adds up the water losses from yesterday and today to generate the target water intake for tomorrow.
YESTERDAY
Calculate the fluid deficit, or the water that the patient has already lost to get to their current sodium. First, determine how much sodium is elevated relative to target (as a percentage):
(Current Na – Target Na)/Target Na
Multiply that by the total body water. 60% body water for lean/younger men, 50% for lean/younger women and older men, and 40% for obese men and women. The full formula for water deficit:
(% Body Water x Body Weight) x [(Current Na – Target Na)/Target Na]
TODAY
Calculating the ongoing fluid losses and how much free water the patient is losing daily as you replete.
Pearl: For first 1L urine , ignore. For urine output (UOP) between 1-3L, assume half of this UOP is lost free water. Assume all UOP beyond 3 L is completely lost as free water. Check out this Curbsiders podcast on hypernatremia.
The more precise method is the electrolyte free water clearance:
Free Water Clearance = Urine volume x [1- (Urine Na + Urine K) ]/ serum Na)
TOMORROW
Add “Yesterday” and “Today” to find the target water intake for “Tomorrow.” Divide the target water intake by 24 hours and replace hourly as oral free water (preferred) or intravenous free water (with dextrose) if the patient is unable to drink or does not have enteral access. NOTE, large volumes of intravenous 5% dextrose and water infusions may cause an osmotic diuresis (through hyperglycemia) and worsen renal water losses.
For certain cases of hypernatremia, there are specific therapies as follows.
- Central DI: Desmopressin (DDAVP), either intranasal, intravenous, or subcutaneous.
- Nephrogenic DI:
- Thiazide diuretics: thiazides induce mild hypovolemia which increase proximal tubular reabsorption of sodium and water causing decrease in distal delivery of water to the ADH-sensitive sites in the collecting tubules and reducing the urine output improving polyuria. Also, thiazide increase expression of AQP2 in the collecting duct enhancing water reabsorption.
- Acetazolamide – blocking carbonic anhydrase activates tubular glomerular feedback lowering GFR to decrease urine output despite a lack of ADH activity.
Take Home Messages
- Hypernatremia is always hypertonic, there is no such thing as “pseudohypernatremia.” If patients have access to and the desire to drink water, they will be able to protect themselves from hypernatremia – even in the total absence of ADH.
- In almost all cases, hypernatremia is due to loss of water from the body (renal or extra-renal).
- Standard text books suggest to correct sodium no faster than 10 mEq/L per day, but retrospective data and case reports cannot find any evidence that breaking this speed limit causes any patient harm.


Great discussion, and very nice review for hypernatremia
Tomorrow’s replacement may overcorrect if the underlying cause is corrected?
nice case and good approach
Excelente información, todo está siendo muy útil para aplicar en pacientes, muchas gracias y felicidades por su conocimiento y compartir