PART 4: CONTROL ISSUES
1. Losing Control:
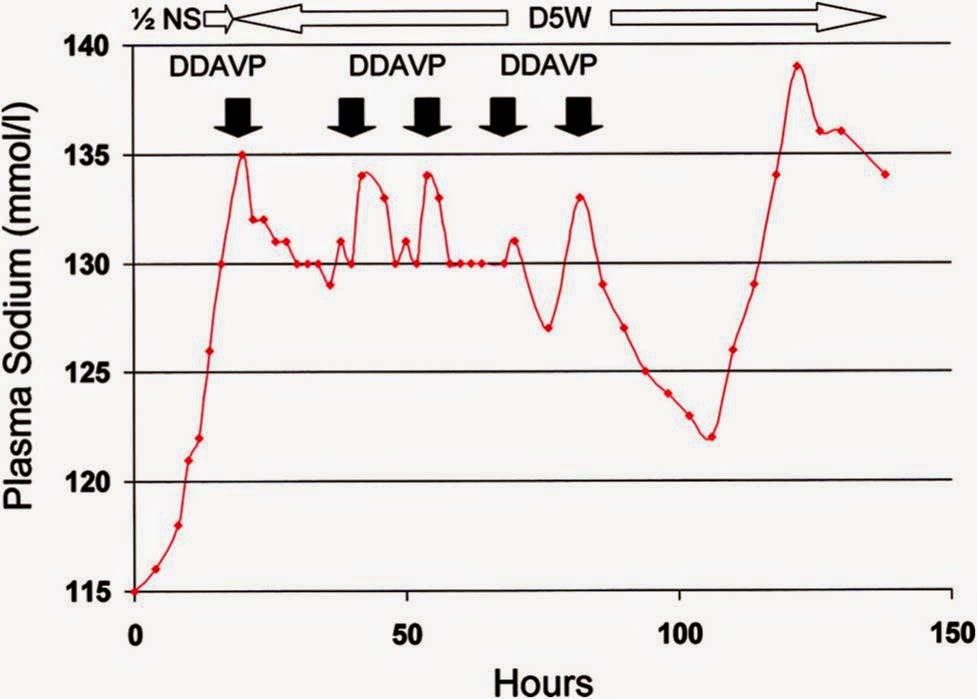
In the preceding posts, I explained how sudden emergence of water diuresis as
the predominant mechanism by which rapid overcorrection of serum sodium happens
in cases of severe chronic hyponatremia.
Few situations or more stressful in nephrology than when we suddenly
find that serum sodium has increased by 12 mmol or more within a few hours. The usual scurried response is the immediate
administration of 5% dextrose water, DDAVP are both. There has recently been
some evidence that using DDAVP with D5W rapidly re-lower the sodium is well
tolerated. But, as it was illustrated in this
paper, the response to these therapies is very unpredictable with the usual
clinical course being a rather erratic series of rises and falls in serum sodium.
In the preceding posts, I explained how sudden emergence of water diuresis as
the predominant mechanism by which rapid overcorrection of serum sodium happens
in cases of severe chronic hyponatremia.
Few situations or more stressful in nephrology than when we suddenly
find that serum sodium has increased by 12 mmol or more within a few hours. The usual scurried response is the immediate
administration of 5% dextrose water, DDAVP are both. There has recently been
some evidence that using DDAVP with D5W rapidly re-lower the sodium is well
tolerated. But, as it was illustrated in this
paper, the response to these therapies is very unpredictable with the usual
clinical course being a rather erratic series of rises and falls in serum sodium.
Two mechanisms are responsible for the vast majority of cases
of overcorrection due to emergence of water diuresis. (1) a sudden drop in plasma ADH/AVP levels
due either to resolution of a transient source of ADH secretion or repletion of
subclinical hypovolemia and (2) in cases of solute depletion hyponatremia, the
sudden availability of solute (in the form of saline solutions or protein load)
in the setting of an appropriately suppressed ADH. The common feature of both these phenomena is
the very low level of plasma ADH which allows water diuresis.
of overcorrection due to emergence of water diuresis. (1) a sudden drop in plasma ADH/AVP levels
due either to resolution of a transient source of ADH secretion or repletion of
subclinical hypovolemia and (2) in cases of solute depletion hyponatremia, the
sudden availability of solute (in the form of saline solutions or protein load)
in the setting of an appropriately suppressed ADH. The common feature of both these phenomena is
the very low level of plasma ADH which allows water diuresis.
2. Gaining Back the
Control: So how can we prevent the
sudden water diuresis which is the hallmark of serum sodium overcorrection?
We’ve argued above that the lack of sufficient ADH or sudden turning off of the
ADH secretion is responsible for the sudden loss of free water in the urine. To
address this issue specifically, in this paper by Sood et al, the Rochester group tested a very simple yet brilliant idea: why
not keep the SIADH state from turning off by creating a robust iatrogenic state
of SIADH? This was achieved by giving IV DDAVP 2mg every 8 hours (1 mg was
tried as well but there was some breakthrough diuresis; also q6hr schedule was
also tried). What this does is, by greatly reducing urine output, stabilize the
denominator in Edelman’s equation (i.e. almost eliminated changes in TBW, see
figure in previous post) and turn the patient into the proverbial beaker, into
which now sodium, potassium and water can be added as needed to control the
rate of sodium correction. In their series of 25 patients with starting serum
sodium of less than 120 mEq/L, quoting directly from the abstract, “Mean
changes in serum sodium levels during the first and second 24 hours of therapy
were 5.8 +/- 2.8 (SD) and 4.5 +/- 2.2 mEq/L, respectively, without correction
by >12 mEq/L in 24 hours or >18 mEq/L in 48 hours and without a decrease
during therapy.” There was no difference in the predicted and actual correction
of sodium and there were no adverse effects associated with the treatment.
Control: So how can we prevent the
sudden water diuresis which is the hallmark of serum sodium overcorrection?
We’ve argued above that the lack of sufficient ADH or sudden turning off of the
ADH secretion is responsible for the sudden loss of free water in the urine. To
address this issue specifically, in this paper by Sood et al, the Rochester group tested a very simple yet brilliant idea: why
not keep the SIADH state from turning off by creating a robust iatrogenic state
of SIADH? This was achieved by giving IV DDAVP 2mg every 8 hours (1 mg was
tried as well but there was some breakthrough diuresis; also q6hr schedule was
also tried). What this does is, by greatly reducing urine output, stabilize the
denominator in Edelman’s equation (i.e. almost eliminated changes in TBW, see
figure in previous post) and turn the patient into the proverbial beaker, into
which now sodium, potassium and water can be added as needed to control the
rate of sodium correction. In their series of 25 patients with starting serum
sodium of less than 120 mEq/L, quoting directly from the abstract, “Mean
changes in serum sodium levels during the first and second 24 hours of therapy
were 5.8 +/- 2.8 (SD) and 4.5 +/- 2.2 mEq/L, respectively, without correction
by >12 mEq/L in 24 hours or >18 mEq/L in 48 hours and without a decrease
during therapy.” There was no difference in the predicted and actual correction
of sodium and there were no adverse effects associated with the treatment.
Essentially, by converting the patients into human
“beakers” by inducing iatrogenic SIADH and then infusing 3% saline at
the desired rate allow for safe and predictable rise in serum sodium without
any complications.
“beakers” by inducing iatrogenic SIADH and then infusing 3% saline at
the desired rate allow for safe and predictable rise in serum sodium without
any complications.
Our experience with this protocol has been extremely
gratifying. When this protocol was used
very carefully, the serum sodium correction graph was almost invariably an
almost straight line: Something that we almost never see with the traditional
method of treatment of severe hyponatremia.
gratifying. When this protocol was used
very carefully, the serum sodium correction graph was almost invariably an
almost straight line: Something that we almost never see with the traditional
method of treatment of severe hyponatremia.
Once a serum sodium is between 125 and 130 mmol/L DDAVP can be
discontinued while closely watching the patient.
discontinued while closely watching the patient.
There are a few important points that need to be mentioned
here.
here.
#1 — It has to be clarified to the nursing staff that the
DDAVP needs to be given exactly every 8 hours and the dose cannot be
missed. If the dose is missed, there can
be breakthrough large volume diuresis in about 10-12 hours from the last dose
which can cause overcorrection.
DDAVP needs to be given exactly every 8 hours and the dose cannot be
missed. If the dose is missed, there can
be breakthrough large volume diuresis in about 10-12 hours from the last dose
which can cause overcorrection.
#2 — The water content of all fluids given/ingested will be
retained. Therefore a very strict fluid
restriction needs to be enforced. In the
IV fluids being given to the patient’s in the form of infusions with
antibiotics etc. need to be accounted for by calculation.
retained. Therefore a very strict fluid
restriction needs to be enforced. In the
IV fluids being given to the patient’s in the form of infusions with
antibiotics etc. need to be accounted for by calculation.
#3 — in patients with congestive heart failure lasix can be
used if it seems like fluid overload is becoming a problem.
used if it seems like fluid overload is becoming a problem.
#4 — if a double-lumen PICC line is being used for 3% saline
infusion and for drawing labs, the hypertonic infusion should be held for a few
minutes before a drawing serum sodium level.
Recirculation can give a falsely elevated sodium level. An important clue in this situation would be
that there would be no large change in urine output that would be expected with
a true sudden rise in serum sodium.
infusion and for drawing labs, the hypertonic infusion should be held for a few
minutes before a drawing serum sodium level.
Recirculation can give a falsely elevated sodium level. An important clue in this situation would be
that there would be no large change in urine output that would be expected with
a true sudden rise in serum sodium.
This protocol is somewhat opposite of what we have
traditionally been taught regarding treatment of severe hyponatremia. Given how stress-free and easy the management
of severe hyponatremia has become with this for me and other colleagues, I
expect this protocol to gain more widespread acceptance over the next few
years. I would also like to know if
anybody has had experience with this protocol, good or bad.
traditionally been taught regarding treatment of severe hyponatremia. Given how stress-free and easy the management
of severe hyponatremia has become with this for me and other colleagues, I
expect this protocol to gain more widespread acceptance over the next few
years. I would also like to know if
anybody has had experience with this protocol, good or bad.
Hyponatremia remains a clinical challenge but is also fun and
stimulating at the same time. A little
time spent on determining the physiology at work and using more quantitative
methods of choosing the doses of 3% saline coupled with good results for the
patient make it very rewarding as well.
stimulating at the same time. A little
time spent on determining the physiology at work and using more quantitative
methods of choosing the doses of 3% saline coupled with good results for the
patient make it very rewarding as well.
Posted by Hashim Mohmand


Ashraf: interesting question. I've never encountered such a case where chronic severe hyponatremia needed correction in an active-CVVHD case. So many variables in such a situation but the dialysate composition is often difficult to change and the need for clearance will also play into the dialysate flow rates.
However, I'm assuming that most such patients will be anuric or oliguric which will take the major variable of urine output out of the picture.
I'm guessing that in such a patient, I would bolus for initial rapid correction or 2-4 mEq/L for symptoms but check Na very frequently the first few hours to see how the dialysis is affecting Na concentration and then titrate 3% saline accordingly. I would probably check Na hourly for the first 3-4 hours to make sure there are no sudden fluctuations and then q2-3 hr for sometime thereafter.
Great post. I am curious to know your approach to severe hyponatremia in the setting of CRRT. How do you safely provide CVVHD or CVVHDF without overcorrection.
thank you dear Hashim Mohammed for making Hyponatremia management so much more clear and concise. Really enjoyed all your articles. Thank you for sharing your knowledge. Looking forward for more articles from you
Thank you for those clear and concise articles.