 This is probably fairly basic to many renal fellows already, but the Hemodialysis Prescription is an integral part of any nephrologist’s routine.
This is probably fairly basic to many renal fellows already, but the Hemodialysis Prescription is an integral part of any nephrologist’s routine.
The hemodialysis prescription should specify the following:
1. The dialyzer being used. These days, most dialysis units are using high-flux dialyzers in order to improve middle-molecular clearance.
2. The time on dialysis. This generally ranges anywhere between 2.5 to 4.5 hours, though there are patients who will require more or less dialysis than this. Increasing the time on dialysis is probably the single-most important change that can be made in order to increase the efficiency of dialysis.
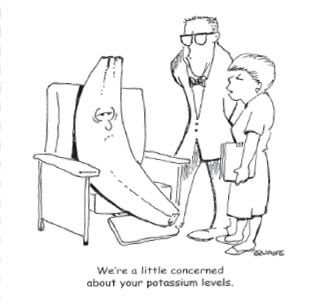
3. The potassium bath concentration. I was taught the “Rule of 7’s”: the patient’s K plus the dialysate bath K should equal approximately 7. For example, if somebody presents with a K of 5.2, put them on a 2 K bath; if they present with a K of 3.3, put them on a 4 K bath. The lowest K bath I’ve ever used is a 1 K bath and I don’t think there’s any reason to use anything higher than a 4K bath.
4. The calcium bath concentration. More recently the trend has been to use a Ca bath which is slightly lower than physiologic concentrations–2.5 mEq/l–in order to minimize the risk of vascular calcification which is thought to accelerate cardiovascular disease. Patients with hypercalcemia may be placed on a Ca bath of 2, and patients who are immediately status-post parathyroidectomy should be placed on a Ca bath of 3 or 3.5 to avoid symptomatic hypocalcemia from “hungry bone syndrome.”
5. The Blood Flow (Qb). We often write for a blood flow rate of “best” which is ideally between 400-450 cc/min, though ultimately it’s the dialysis nurse who will determine the optimal rate of flow, as not all fistulas or catheters are able to sustain such high flows. The higher the flows, the better the clearance. Patients just starting out on dialysis should be run with a lower Qb (e.g., 250 cc/min) which is gradually increased over the course of the first 3 sessions.
6. The Dialysate Flow (Qd). The rate of dialysate flow can be easily varied but plays a relatively minimal role in the determination of clearance efficiency. We typically use a Qd of 500 cc/min when somebody is initiating on dialysis and a Qd of 800 cc/min for an established dialysis patient.
7. Address Anemia. This should include whether the patient meets requirements for Epogen or iv iron therapy.
8. Address Bone Metabolism. This should include addressing the patient’s calcium, phosphorus and PTH levels; whether they are on the appropriate dose of phosphate binders, and whether they need any pharmacologic titration of their PTH level in the form of calcitriol, vitamin D analogues, or cinacalcet.
9. Any additional medications which need to be given at dialysis (e.g., antibiotics) should also be addressed.
10. Any dialysis-related complications (e.g., intradialytic hypotension, cramping, etc) should also be addressed.


what if I need to keep Na levels higher 145- 150?
why do we add calcium and potassium in acid jar not in bicarbonate jar?
Guidelines recommend low Ca baths for treatment of refractory hypercalcemia. Is there a proven risk of developing arrhythmias from rapid correction of hypercalcemia (analogous to pro-arrhythmic risk of too rapid correction of hyperkalemia)?
How do we increase the dialysate calcium concentration?
Can we add galcium gluconate to the acid jar?
what will be the quantity to be added?