 I saw an interesting case yesterday. A 71 year old male, CKD III with a syndrome suggestive of chronic tubulointerstitial disease (U/A trace proteinuria only, disproportionate anemia, mild cortical thinning on ultrasound, normal-appearing vasculature on ultrasound). He had longstanding, intermittent flank pain which began in his 50’s, ascribed to nephrolithiasis, although no stone was ever seen. Anyway, after some probing, he admitted to taking a drug called Vanquish regularly (i.e. daily for over 20 years). I had to look it up, but it turns out to be a compound analgesic (acetaminophen, aspirin and caffeine). I was surprised, as I thought these compounds were off the market, as they are in Europe. So beware, analgesic nephropathy is alive and well in 2009!
I saw an interesting case yesterday. A 71 year old male, CKD III with a syndrome suggestive of chronic tubulointerstitial disease (U/A trace proteinuria only, disproportionate anemia, mild cortical thinning on ultrasound, normal-appearing vasculature on ultrasound). He had longstanding, intermittent flank pain which began in his 50’s, ascribed to nephrolithiasis, although no stone was ever seen. Anyway, after some probing, he admitted to taking a drug called Vanquish regularly (i.e. daily for over 20 years). I had to look it up, but it turns out to be a compound analgesic (acetaminophen, aspirin and caffeine). I was surprised, as I thought these compounds were off the market, as they are in Europe. So beware, analgesic nephropathy is alive and well in 2009!Analgesic nephropathy is a slowly progressive form of kidney disease characterized by polyuria and renal colic (due to papillary ischemia and necrosis) in the early stages, progressing to tubulo-interstitial disease, transitional cell carcinoma and ESRD over many years. It became a rare diagnosis following the removal of phenacetin from analgesic mixtures in the 80’s, but still accounted for 10% of ESRD cases in Australia in 1990.
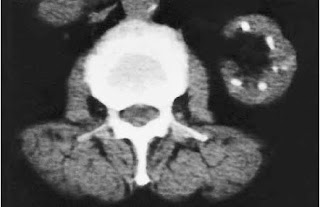
Phenacetin, whose main metabolite is acetaminophen, was originally believed to be the cause. But this was challenged by the appearance of cases where phenacetin was not involved. The modern definition of analgesic nephropathy does not mention phenacetin: “a slowly progressive disease resulting from the daily use for many years of mixtures containing at least two anti-pyretic analgesics and usually caffeine or codeine (or both), which may lead to psychological dependence”. The diagnosis is made based on pathgnomic appearances on non-contrast CT (reduced renal size, bumpy contours and papillary calcifications) in the appropriate clinical context.
Phenacetin, whose main metabolite is acetaminophen, was originally believed to be the cause. But this was challenged by the appearance of cases where phenacetin was not involved. The modern definition of analgesic nephropathy does not mention phenacetin: “a slowly progressive disease resulting from the daily use for many years of mixtures containing at least two anti-pyretic analgesics and usually caffeine or codeine (or both), which may lead to psychological dependence”. The diagnosis is made based on pathgnomic appearances on non-contrast CT (reduced renal size, bumpy contours and papillary calcifications) in the appropriate clinical context.

