Similar to my recent post on C1q Nephropathy, IgM Nephropathy (IgMN) is a podocytopathy that is often considered a variant of Minimal Change disease (MCD) or FSGS. Like C1QN, it is also a controversial entity with a lack of uniformity from a diagnostic point of view. This undoubtedly leads to under-reporting with some pathologists calling a case IgMN what others would call MCD/FSGS/Mesangial Proflierative GN with low level IgM staining.
First descriptions of IgMN reported mesangial hypercellularity on light microscopy, granular IgM and C3 mesangial deposits on immunofluorescence with electron dense deposits in about half of cases. Podocyte foot process effacement was also evident consistent with the presentation of nephrotic syndrome. The incidence has been reported to be 2-18% of renal biopsy series and age at presentation appears to be bimodal with a peak in childhood and again later in life, 6-7th decades. The incidence of IgMN may be higher in the developing world and most recent reports come from developing nations (ref, ref).
The accurate diagnosis of IgMN is important from a prognostic and therapeutic point of view. Overall, IgMN does not respond to steroids as well as MCD with a higher proportion of patient with steroid-dependent and resistant disease. Furthermore, assessment of children with steroid-dependent and resistant MCD revealed a high proportion of IgMN, which appeared to respond better to cyclosporin than to cyclophosphamide. Rituximab (as ever!) may be another alternative therapeutic choice, although evidence remains at case report level, including a case of recurrent IgMN post-transplant. Similar to C1QN, the severity is likely dependent on the light microscopic changes with MCD patterns reporting an excellent remission rate and an FSGS pattern of injury having a worse prognosis (ref). Most cases however may have mesangial proliferative changes evident. There is even a report of IgMN presenting with crescentic lesions.
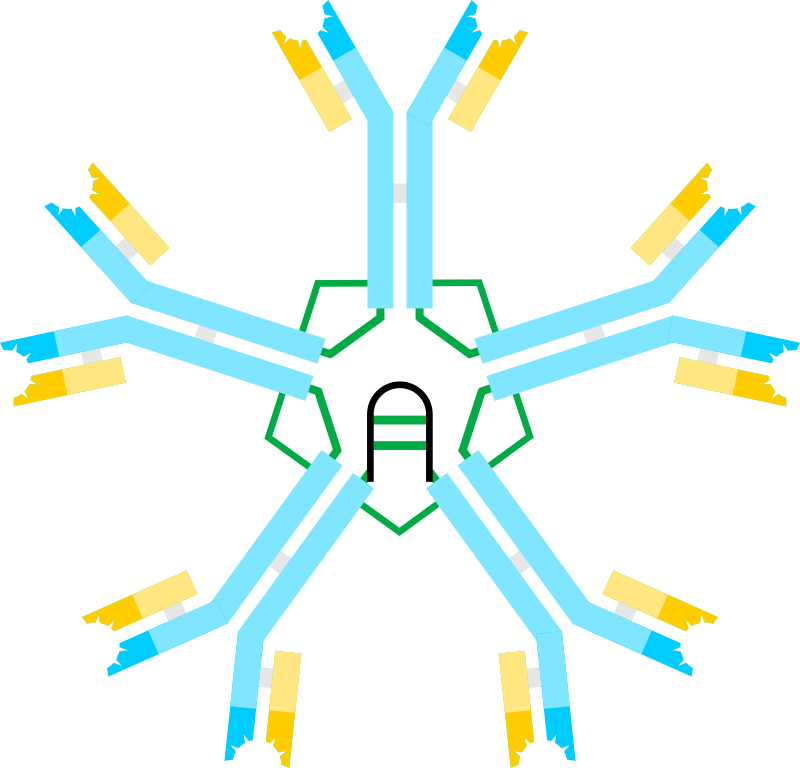
IgM deposition may be seen in many other glomerular disorders and its role is unclear. Is it an innocent bystander, reflecting natural IgM binding to exposed epitopes on injured glomerular cells? There is some evidence that IgM deposition may activate complement and that efforts to prevent IgM antibody deposition may prevent complement activation and slow the progression of glomerular injury. IgMN is another glomerular disease that we have an unclear understanding of pathogenesis and etiology where we rely on crude pathological descriptions. Hopefully the future will bring clarity to these diseases and facilitate precise molecular diagnosis of entities such as IgMN.