This is a fictional case, designed for educational purposes
The Case
The patient is a 66 year-old with a history of hypertension who presented with complaints of fatigue and recurrent “sinus infections” over the past few months. He had been treated with 2 different antibiotics in the prior month and occasionally used ibuprofen.
His home medications included amlodipine, hydrochlorothiazide (HCTZ), and metoprolol. Blood chemistries and urinalysis (UA) were sent and the patient was soon advised to go to the Emergency Department (ED). His labs revealed blood urea nitrogen (BUN) 164 mg/dL, creatinine 12.95 mg/dL, K 5.9 meq/L, bicarbonate 14 meq/L, and serum albumin 3.9 g/dL.
The Urine
Urinalysis revealed specific gravity (SG) 1.009, 2+ protein, 3+ blood. The laboratory microscopy reported 5-10 white blood cells (WBCs) / high power field (hpf) and > 50 red blood cells (RBC)/hpf.
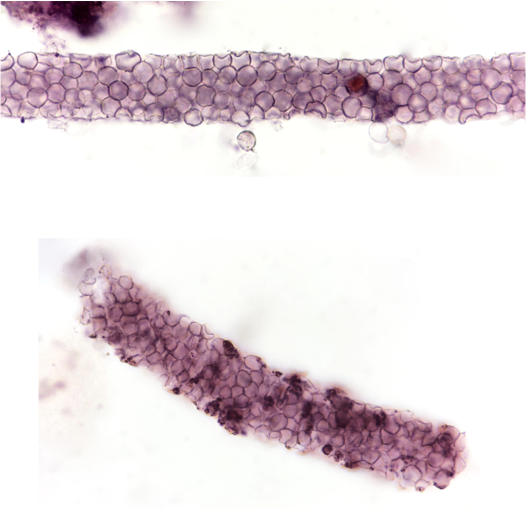
Let’s look into the microscope…
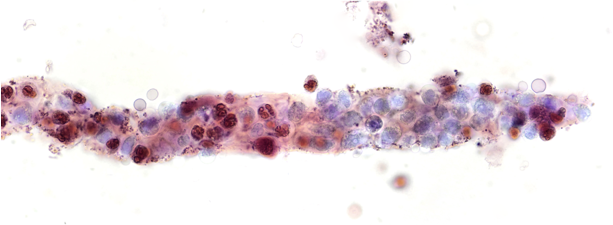
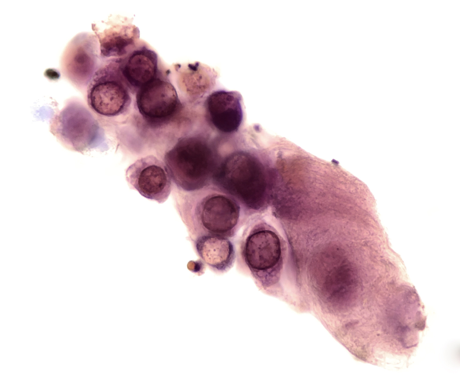

While these (and hematuria) may be seen in severe acute interstitial nephritis the history and findings were most concerning for an acute proliferative glomerulonephritis (GN) and a kidney biopsy was scheduled. Antibody titers including anti-glomerular basement membrane (GBM), proteinase-3 (PR3), myelopyroxidase (MPO) anti-nuclear antibody (ANA) and complement levels were normal.
The Kidney Biopsy
* Necrotizing and Crescentic GN with linear IgG staining consistent with Anti-GBM disease
* Severe interstitial edema
* Acute tubular injury
Take Home Messages:
* WBC casts may be a prominent feature in acute proliferative GNs
* RTEC casts imply the presence of acute tubular injury
* Mixed cellular casts may be a frequent finding in acute proliferative GNs
* RBC casts are usually indicative of glomerulonephritis or vasculitis
* Absence of an anti-GBM antibody on serologic screening does not exclude the possibility of anti-GBM disease
Post by: Jay Seltzer, MD



Atypical antiGBM disease