John Henry Dasinger, PhD
Postdoctoral Fellow
Augusta University
George Bernard Shaw, Irish playwright and Nobel Prize winner, said it best,
“There is no love sincerer than the love of food“
George Bernard Shaw
In the current coronavirus infectious disease 2019 (COVID-19) pandemic, many of us may have turned to food to bring us comfort in these trying times. Social media accounts have been filled with pictures of new bakes and recipes tried for the first time. While these new recipes brought you some comfort, I hope that you were able to try some new recipes of your favorite vegetables as well, since plant-based dietary patterns could help with long-term health. This could be particularly important for those who have chronic kidney disease (CKD), specifically for women of childbearing age. Here we’ll discuss the potential role of dietary modification and the impact this can have on CKD progression.
CKD continues to be a global health burden, affecting about 10% of the world’s population. While there is no cure for the progression of CKD, dietary management is considered one modifiable factor to potentially slow disease progression. This could be approached in one of two ways:
1) decreasing total dietary protein content or
2) altering the source of dietary protein.
Protein content- In a recent prospective study of nearly 10,000 healthy subjects, Jhee et al investigated the association between dietary protein content (based on food frequency questionnaire) and estimated glomerular filtration rate (eGFR). The authors reported that baseline parameters for study subjects were an eGFR of 93.9 ± 14.1 mL/min/1.73m2 with mean daily protein intake of 1.1 ± 0.5 g/kg/day. These subjects were then categorized into four quartiles based on daily protein intake, and followed for about 11 years after baseline measurements were made. The authors found that those subjects who ingested the highest amounts of daily protein intake (1.7 ± 0.6 g/kg/day) had a higher odds ratio for the decline in eGFR over time compared to the lowest quartile of daily protein intake, upon full adjustments for confounding variables (OR=1.32, 95%CI 1.02-1.73). Interestingly, when subjects were further divided into a subgroup based on hyperfiltration status, rate of eGFR decline was greater in the highest protein intake group with evidence of hyperfiltration (-3.1 ± 2.8 mL/min/1.73m2/year) versus those without hyperfiltration (-2.1 ± 2.6 mL/min/1.73m2/year). From this data, a relationship between high daily protein content and more rapid kidney function decline was demonstrated. This study highlights the potential importance of dietary protein content in the progressive loss of kidney function.
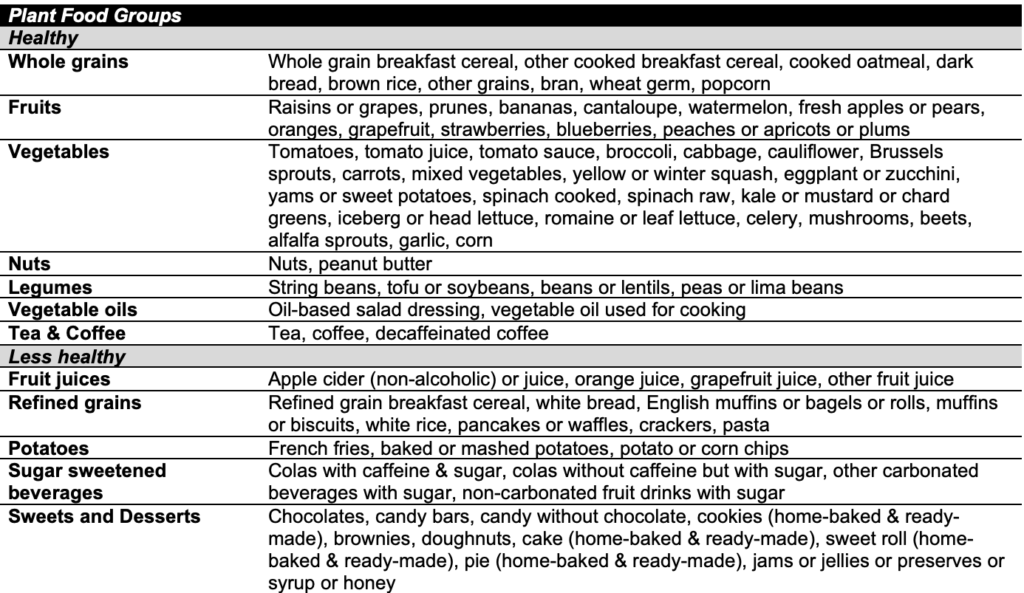
Altered protein source- The source of dietary protein can also have an impact on kidney function. A protective effect has been proposed for plant-based dietary protein, which has been thoroughly reviewed by Kamper et al. A meta-analysis of 18 cohort studies including over 600,000 subjects concluded that a diet rich in whole grains and vegetables, and lower intake of red or processed meats was associated with a lower odds of incidence of CKD (OR=0.70, 95% CI 0.60-0.82) and albuminuria (OR=0.77, 95% CI 0.59-0.99) over an average of 10 years of follow-up. Furthermore, Kim et al performed a study evaluating how a plant-based diet can impact the incidence of CKD over a 20 year period in over 15,000 subjects in the Atherosclerosis Risk in Communities (ARIC) study. Using the semiquantitative Willett food frequency questionnaires, subjects were placed into quintiles based on dietary intake of healthy plant foods, less healthy foods and animal foods, as shown in Table 1. This study demonstrated that the highest consumption of a plant-based diet was associated with a lower CKD risk (25% lower risk) and a slower annual decline in eGFR (-1.54 mL/min/1.73m2) relative to the group of subjects that consumed the lowest amount of vegetables. Together, these studies suggest that a diet rich in vegetables could be a healthy option for your kidneys. Perhaps, I actually should have listened to my parents and eaten my vegetables more frequently as a child!
If these associations between dietary habits and kidney health hold true, they could have major implications for patients with CKD.
Is there any relationship between protein intake and pregnancy? In a normal pregnancy, it is suggested that protein intake should increase throughout pregnancy by 1 g/day during the first trimester, 8 g/day in the second and 23-29 g/day in the third to meet the metabolic demands of the growing fetus. This increase in protein intake throughout pregnancy might be difficult in women with CKD due to the impairment in renal function. It is known that women who are diagnosed with CKD have worse maternal (e.g. preterm delivery, preeclampsia and maternal death) and neonatal (e.g. low birth weight, small for gestation and infant death) outcomes compared to women without CKD. Additionally, the physiological stresses of pregnancy have been observed to result in an acceleration of kidney disease progression. Imbasciati et al reported that eGFR declines 1.17 mL/min per month in pregnant women with CKD, relative to a pre-pregnancy reduction of only 0.20 mL/min per month. Can dietary protein source help lessen the risk for adverse maternal outcomes such as preeclampsia in women with CKD?
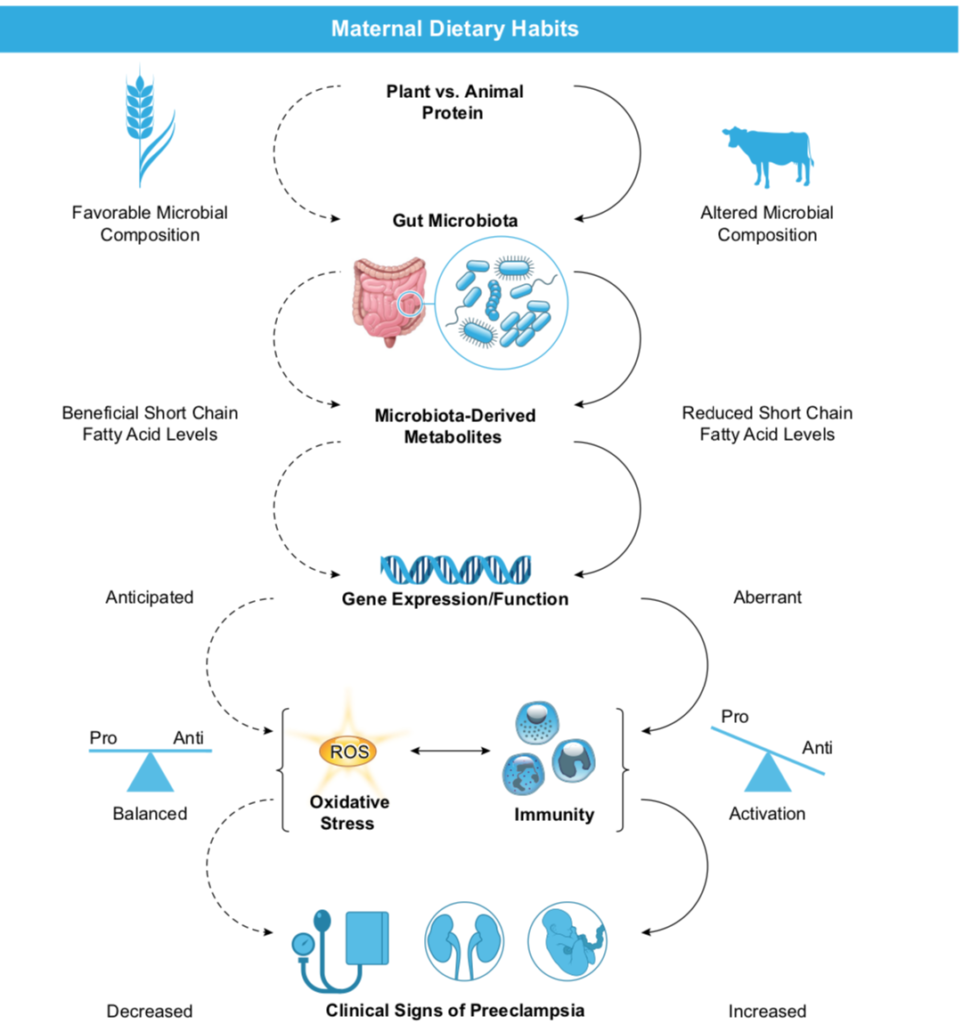
Dietary protein source- In terms of using diet as a therapeutic approach, there are several association studies demonstrating the protective effects of dietary protein content and source. In two small cohort studies of women with CKD, it was demonstrated that by maintaining a vegetarian based, moderately protein restricted diet of 0.6-0.7 g/kg/day with increasing daily protein intake throughout pregnancy resulted in no major side effects in the maternal phenotype, such as early preterm delivery. Rather, this intervention was found to decrease the number of small for gestational age babies relative to the control CKD group, who had no dietary restrictions. While there are limited studies on this topic, there are promising data for the use of vegetarian or vegetable-based dietary habits for kidney health, particularly for pregnant women with CKD or women with CKD who are considering pregnancy. Meta-analysis and cohort data demonstrate an approximate 40% increase in risk of developing a hypertensive disorder of pregnancy such as preeclampsia in women with CKD compared with women without CKD. Since preeclampsia and CKD have similar phenotypic characteristics such as hypertension, proteinuria and impaired kidney function, perhaps dietary consumption could be important in both of these diseases as well. The exact mechanisms for why a plant-based diet is protective in CKD are unclear, but the flow chart (Figure 1) can give some insight into the pathways involved in this protection in the context of preeclampsia specifically. Just a little food for thought.
Reviewed by: Elinor Mannon, Tanecia Mitchell, PhD, Matthew Sparks, MD, FASN, FAHA
If you enjoyed reading this post and would like to learn more about diet and its implications for kidney health and disease, consider checking out these other posts on RFN:
Oxalate nephropathy: innocent bystander or primary driver of CKD
Nephrotoxicity of Dietary Supplements and Alternative Medicine



This is an excellent overview of some of the literature around nutrition in CKD, with respect to protein intake and protein sources. I appreciate the fact that the words potential and association are sprinkled throughout the blog post. However, to the unwary reader, the takeaway message might be that we should advise protein restriction as well as vegetable sources of protein intake. That would be the wrong message.
Firstly, nephrology has been plagued by observational data that has not been replicated or confirmed in subsequent randomized controlled trials.
Secondly nutritional epidemiology is full of observational data that has not been replicated and has been, in fact, often overturned, when randomized clinical trials are done.
Hence, to use observational data in nephrology is a double whammy.
It would be useful to review the randomized clinical trials in this area. Low protein diet does not help retard progression of CKD. There is a trial called the MDRD, which is better known for the GFR formula, but the main trial was on protein restriction. Apart from the fact that it did not help reduce progression, the other aspect was that a low protein diet causes malnutrition. These patients were more likely to die once they started dialysis. See Dr Topf’s blog on that piece of information here http://pbfluids.com/2009/03/comment-on-the-latest-mdrd-article-and-the-state-of-clinical-nephro-research/
This little negative information should perhaps be put in bold letters at the top of this blog post.
People who followed low protein diet got malnourished and were more likely to die on dialysis.
Lastly, one should always be careful in translating lifestyle behavior changes from observational literature. There are many things that go along with behavior and when we link them in an observational study, there is a huge amount of residual confounding and selection bias. Is it the protein intake that drove the outcome results that you see, or is it the kind of person who follows a low protein diet? This post sadly seems to have no understanding about these aspects. Most importantly, there is a huge gap between efficacy and effectiveness. Even if something worked in a carefully done randomized control trial, it would not mean that giving that advice will actually translate into change in behavior.
This comment is given in the form of constructive criticism, and also to make any potential readers be cautious before implementing either a low protein diet or vegetable protein