A 56-year-old kidney transplant recipient due to IgA nephropathy presented to the emergency department with a two day history of fatigue, gross hematuria, and pain over her allograft. She was diagnosed with transplant pyelonephritis and treated with antibiotics immediately. In the following days she became oligo-anuric and her creatinine was rapidly rising.
A urine sediment examination on day 3 revealed extensive hematuria with many ringforms and acanthocytes, as well as multiple dark brown casts (Figure 1). At first glance these appeared to be muddy brown casts. On further inspection their reddish-brown hue (Figure 2) was noted, and RBC remnants were seen in some of them (Figure 3 arrow). The casts were identified as hemoglobin/RBC casts.

Figure 1: Phase contrast, left and bright field, right. Original magnification 400x.
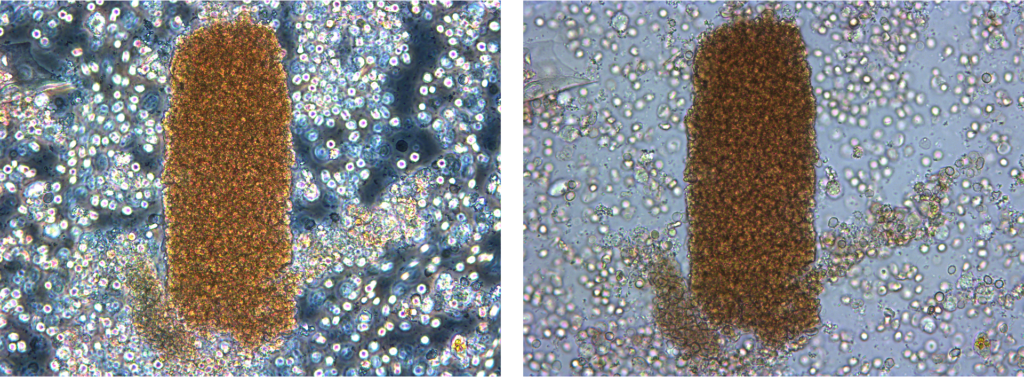
Figure 2: Phase contrast, left and bright field right. Original magnification 400x.
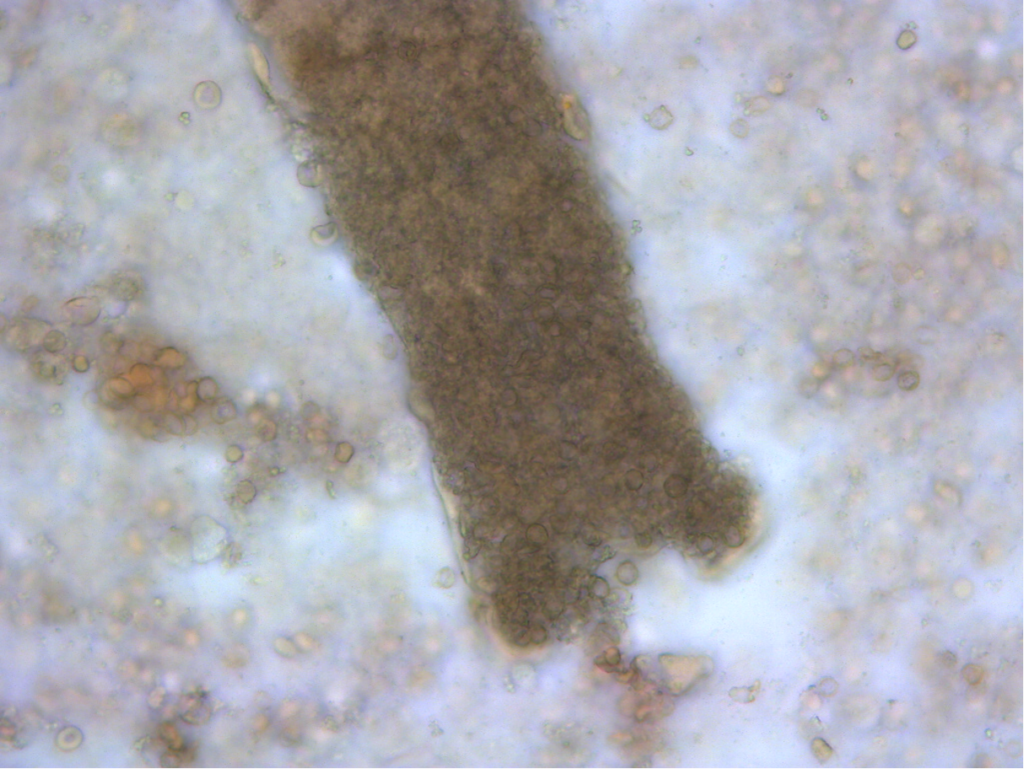
Figure 3: Bright field, original magnification 400x
The patient had a history of IgA nephropathy. Acute renal failure in IgA nephropathy is usually attributed to one of two mechanisms: severe glomerular injury with crescent formation or tubular obstruction/injury by red blood cells due to heavy glomerular bleeding.
Because of dual anti-platelet therapy, a kidney biopsy was contraindicated. Steroids were started because of concerns of RPGN. Two days later, urine output increased suddenly, and kidney function rapidly returned near its baseline.
The acute kidney injury was felt to have been secondary to tubular occlusion by heavy glomerular bleeding.
Edited by: Margaret DeOliveira


