As a general rule, in any patient presenting with acute kidney injury without an obvious cause, obstructive nephropathy must be excluded because prompt intervention can lead to improvement or complete recovery of renal function. Therefore, the detection of hydronephrosis is one of the commonest indications for Point of care renal ultrasonography performed by nephrologists and internists.
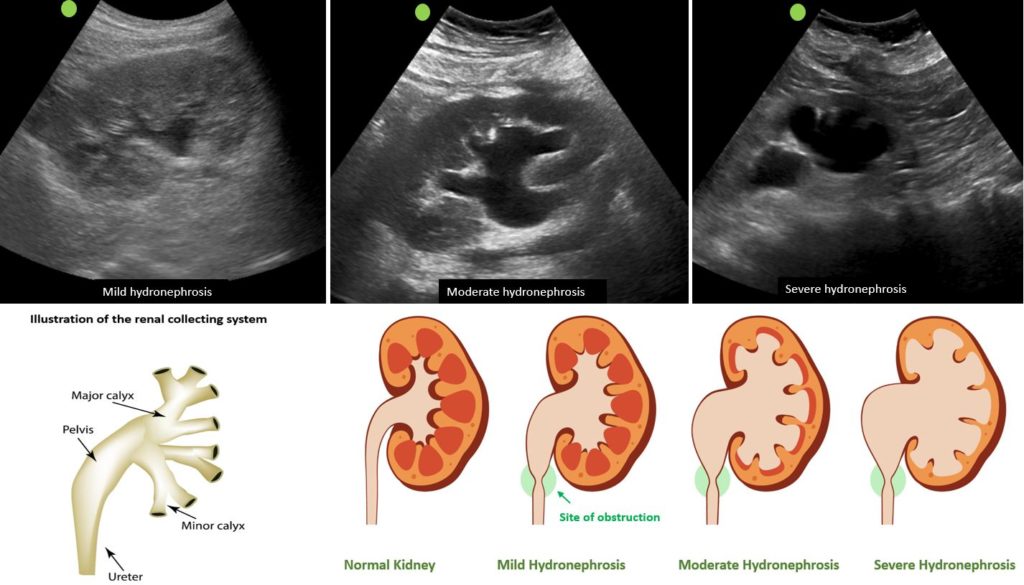
On the sonogram, hydronephrosis appears as branching, interconnected areas of decreased echogenicity (anechoic or black in general, indicating the presence of fluid) in the renal collecting system. The source of obstruction is usually located distal to the kidney, for example, a stone in the pelviureteric junction, ureter or ureterovesical junction or bladder outlet obstruction from enlarged prostate, stone or a mass.
On the other hand, the collecting system of a normal kidney is not well-visualized unless distended and is embedded in the surrounding echogenic sinus fat. The renal pelvis area is hypoechoic but not ‘black’ unless there is hydronephrosis.
As the hydronephrosis increases in severity, the urine moves proximally into the kidney exerting pressure on the parenchyma. While there is no universally accepted grading system, hydronephrosis is often classified as mild, moderate or severe in routine clinical practice.
In mild hydronephrosis, there is dilatation of the renal pelvis and calyces but the pelvicalyceal pattern is retained and the cortex remains unaffected. Distinct medullary pyramids may be seen in some cases though not necessary to make a diagnosis as pyramids are not always appreciable even in a normal kidney.
In moderate hydronephrosis, medullary pyramids start to flatten due to back pressure in addition to dilatation of pelvicalyceal system and outpouching of the calyces, which is sometimes referred to as ‘cauliflower appearance’. Cortical thickness is preserved.
In severe cases, renal pelvis and calyces appear ballooned and cortico-medullary differentiation is lost making the cortex thin. Ultrasound images as well as illustrations demonstrating these grades of hydronephrosis are shown in Figure 1.
In this context, it is important to note that obstructive nephropathy may be missed due to false negative findings in the setting of acute or partial obstruction, volume depletion and retroperitoneal fibrosis. On the contrary, we have to be aware of the false-positive findings, that is conditions that mimic hydronephrosis to avoid any unnecessary and potentially harmful interventions.
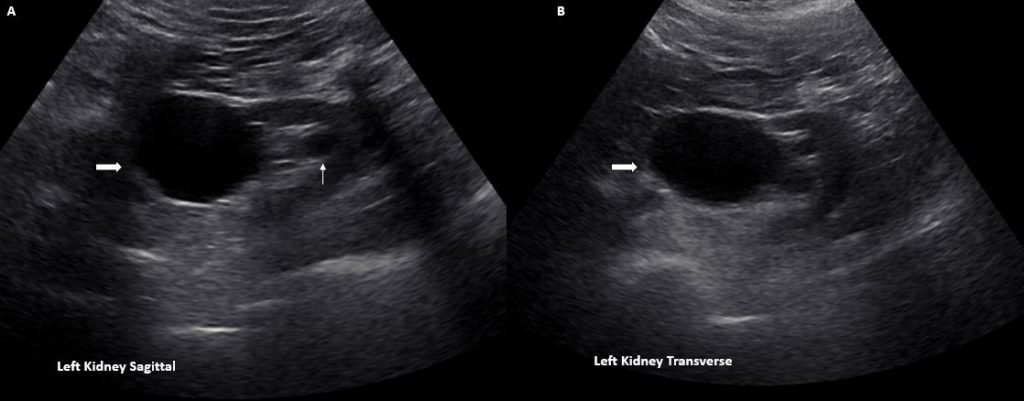
One of these mimics is an extrarenal pelvis. It is an anatomical variant where major portion of the renal pelvis is located outside the renal sinus and is more distensible than an intrarenal pelvis, which is surrounded by sinus fat. On a sonogram, extrarenal pelvis appears as a hypoechoic or anechoic mass just outside the renal sinus and unlike hydronephrosis, it is not associated with dilated calyces, parenchymal thinning, hydroureter, or enlarged kidney per se.
When you see a big ball of fluid ‘outside’ the renal sinus but wonder why the intrarenal collecting system is not dilated from backpressure, think of this entity. Figure 2 demonstrates sagittal (A) and transverse (B) views of the kidney with an extrarenal pelvis filled with urine (thick arrow) without distended calyceal system. A medullary pyramid (line arrow) can be seen just above the central echogenic portion of the kidney suggestive of preserved corticomedullary differentiation and the absence of compression.
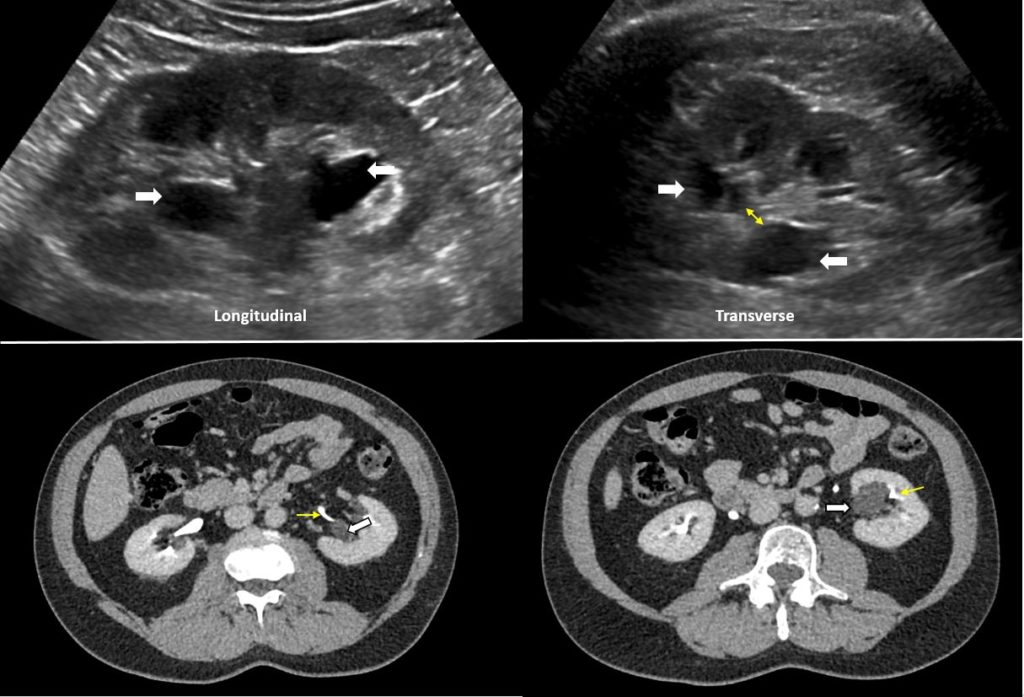
Parapelvic cysts also can mimic hydronephrosis because of their anechoic nature (like urine, clear fluid in the cysts is black on ultrasound) and close proximity to the collecting system. As mentioned above, hydronephrosis appears as branching, ‘interconnected’ anechoic area, while parapelvic cysts are seen as ‘noncommunicating’ renal sinus cystic masses. In addition, a parapelvic cyst is more spherical as opposed to irregular/cauliflower contour of hydronephrosis. When the sonogram is not clear enough, a CT scan with contrast should be considered to differentiate between these two conditions.
Figure 3 demonstrates parapelvic cysts on ultrasound [top panel] appearing as hypoechoic areas in the renal pelvis area. However, note that on the transverse view, these areas do not seem to be connected with one another (double‐headed arrow). Contrast-enhanced CT scan [bottom panel] confirms the diagnosis of parapelvic cysts by showing that these structures (white arrows) are separate from the contrast‐filled collecting system (yellow arrows).
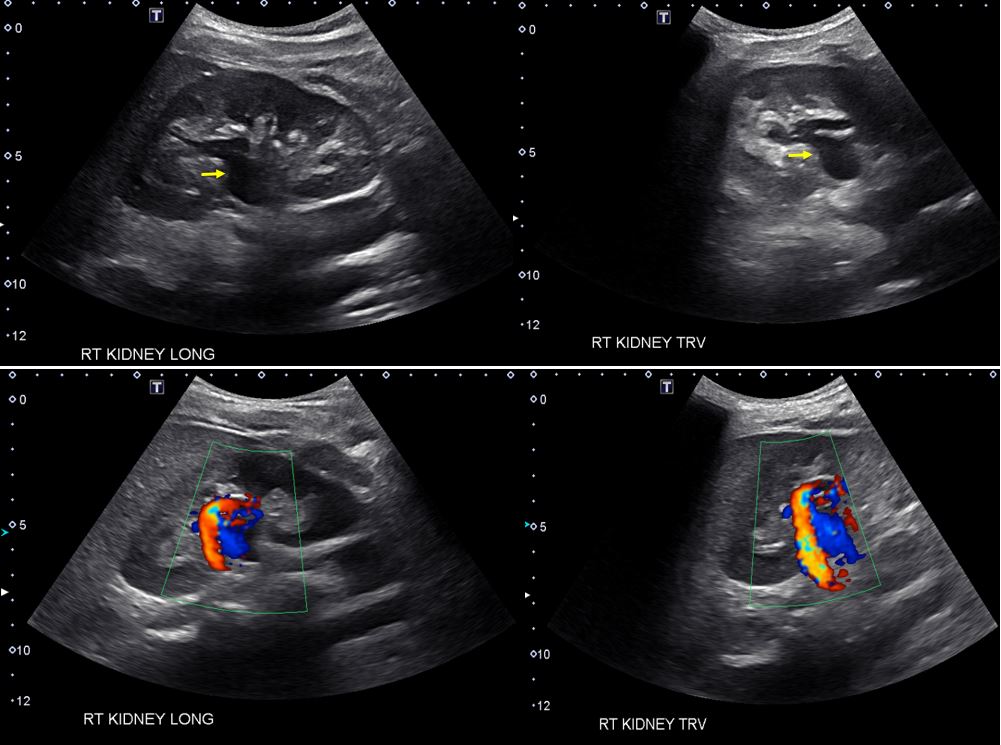
Prominent renal vasculature and vascular malformations can mimic hydronephrosis on grey-scale images because blood also appears black on ultrasound. The simplest way to avoid misdiagnosis is obtaining color Doppler images which demonstrate blood flow if there are vessels in the renal pelvis area.
In fact, we should always obtain a few Doppler images when performing kidney ultrasound irrespective of the suspected etiology. Figure 4 demonstrates anechoic region in the mid‐kidney suggestive of hydronephrosis on grey-scale images [top panel] and color Doppler evaluation of the same area reveals prominent arteriovenous flow suggestive of vascular malformation.
Take-home point: Extrarenal pelvis, parapelvic cysts and vessels in the renal hilum may mimic hydronephrosis on ultrasound. Compare prior imaging studies, obtain color Doppler images and possibly further imaging when applicable for accurate diagnosis.
Abhilash Koratala MD
University of Florida



Very much informative
Very nice informative
Very informative and written without too many medical terms for us lay people! 😀 Definitely gave me more needed information for my urology follow-up appointment next month! I have stage 4 colon cancer and a tumor that cannot be removed because of its vascular and neurological symtomology. It has decided to wrap itself around my left uterer causing me more stress and anxiety. The LAST thing I need right now is a failing kidney!! Keep the good info coming! Cheers!
Informative article. Thank you
Very nice article, enumerating the various causes…
It’s Helpful…
Yet another excellent article on renal POCUS. Thank you for this great series.