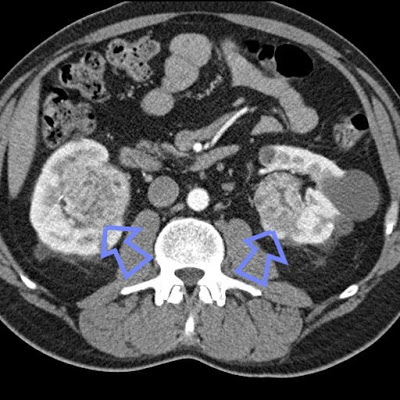
 The case: a 50-ish yo woman, normal baseline renal function, and a history of nephrolithiasis x 2 episodes presented with gross, painless hematuria. She was initially thought to have another stone event, but she had no significant flank pain. Ultimately she underwent CT imaging which revealed bilateral renal masses suspicious for renal cell carcinoma.
The case: a 50-ish yo woman, normal baseline renal function, and a history of nephrolithiasis x 2 episodes presented with gross, painless hematuria. She was initially thought to have another stone event, but she had no significant flank pain. Ultimately she underwent CT imaging which revealed bilateral renal masses suspicious for renal cell carcinoma.
Fortunately, there was no evidence of metastatic disease, and she underwent a R total nephrectomy followed by a partial L nephrectomy, leaving her with about 1/4 of her original nephron mass. Pathology reveals a clear cell-type RCC in both biopsy specimens. Her Cr remains in the 1.0-1.2 range. A question is raised as to why she developed two separate RCC’s.
There is an interesting differential diagnosis of bilateral RCCs which includes some interesting genetic syndromes, the most common of which is von Hippel Lindau Syndrome, an autosomal dominant inherited gene caused by mutations in the VHL gene. Because the VHL gene is a tumor suppressor gene, there are other tumors which may occur in these patients, including pheochromocytomas and hemangioblastomas, among others. Specifically it is the clear cell RCC which occurs in VHL Syndrome. Other genetic disorders causing RCC’s include Hereditary Papillary RCC (caused by mutations in the c-met gene), Tuberous Sclerosis (more likely to cause benign angiomyolipomas, but can result in RCCs), Hereditary Leiomyoma and Renal Cell Cancer Syndrome, and the Birt-Hogg-Dube (BHD) syndrome (resulting in chromophobe RCCs).
Despite these numerous possibilities of mutations causing RCC, a 1998 study revealed that amongst patients with bilateral RCC who underwent extensive mutation screening, only 12% had a hereditary form of RCC whereas the remaining 88% had “sporadic”, bilateral RCCs.