 Much of the clinical year of the renal fellow is spent in the hospital rounding on patients admitted with access malfunction, catheter related infections or are in the ICU’s with acute kidney injury. Many of these patients will require temporary dialysis access that in many cases will be life saving. Nate has already nicely discussed the debate between when to choose the femoral vs. the internal jugular vein in a previous post. These lines have the potential to pose many difficulties as patients with renal failure can have difficult and limited access sites. A difficult line can be avoided with appropriate training and imaging. We are fortunate to have an ultrasound readily available in our dialysis unit for vas-cath placement, but many hospitals do not.
Much of the clinical year of the renal fellow is spent in the hospital rounding on patients admitted with access malfunction, catheter related infections or are in the ICU’s with acute kidney injury. Many of these patients will require temporary dialysis access that in many cases will be life saving. Nate has already nicely discussed the debate between when to choose the femoral vs. the internal jugular vein in a previous post. These lines have the potential to pose many difficulties as patients with renal failure can have difficult and limited access sites. A difficult line can be avoided with appropriate training and imaging. We are fortunate to have an ultrasound readily available in our dialysis unit for vas-cath placement, but many hospitals do not.
An interesting article was published in the Feb 2010 CJASN by Prabhu et al in which 110 patients were randomized into two groups. One group had ultrasound guided femoral catheter placement and one group did not. The results, not surprisingly, showed that patients who had ultrasound guided vas-cath placement had a higher overall success rate (98.2% vs. 80%), better first attempt success rate (85.5% vs. 54.5%) and had few complications (5.5% vs. 18.2%). Furthermore, of the 11 patient who did not have a successful catheter placed without ultrasound guidance, 10 of these had success with use of the ultrasound in the exact same leg. This article also reviewed 3 other studies comparing ultrasound vs. standard landmark techniques. These studies show similar results.
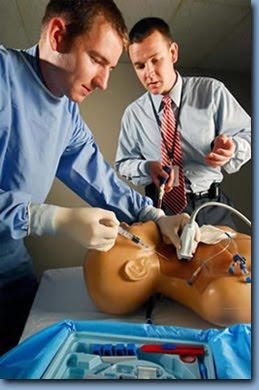
Another interesting article was published in AJKD in 2009 by Barsuk et al from Nothwestern University. This study looked at the use of an ultrasound compatible central line simulator (like on the picture above) and deliberate practice before actually placing lines on patients. Again two groups were assessed in an unblinded fashion.
- Simulator Group- 12 first-year fellows were trained with the simulator and tested before and 2 weeks after the intervention with a 27 item clinical skills examinations checklist (available from the supplementary data).
- Traditional Group- 6 graduating second-year fellows were tested using the simulator once during the last 2 months of their fellowship.
Results from this study also showed benefit using the central line simulator. Interestingly, only one of the six graduating fellows met the minimum passing score. The simulator group improved dramatically from a score of 29.5% to a score of 88.6%. The course was highly rated by the attendees. It would be interesting to see if complications rates went down after the intervention. Also, I wonder if the higher scores would hold up over time. If I took the same test in a 2 week interval, I’m pretty sure I would score much higher on the second attempt. Especially after attending a 2 hour course.
I hope that more nephrology programs begin instituting programs like the simulator course. Likewise, ultrasound guided vas-cath placement needs to become standard practice. This can only help patient care and improve the competency of the graduating fellows. That being said, how many times do nephrologists in private practice put in temporary catheters? As the interventional radiology field continues to grow, this is surely decreasing.


Thanks for the comment. Please let us know when your paper is published. What program is the paper coming out of?
We routinely use US guidance for placement of central lines and dialysis access in our patients. IJ access is only placed under US guidance and femoral is left up to the discretion of the operator. We are in the process of publishing data in CHEST that demonstrates the effectiveness and safety of US training for PGY-1 through 3 level house staff. I agree that this will likely become standard of care in the near future.