Recently one of our patients had been having trouble with her AVF. She had it for 9 years and had multiple previous revisions and angioplasties of recurrent subclavian and brachiocephalic stenoses. She was admitted for insertion of a bovine interposition graft and the following day she had a tunneled RIJ catheter inserted as a bridge until the AVF could be used again.
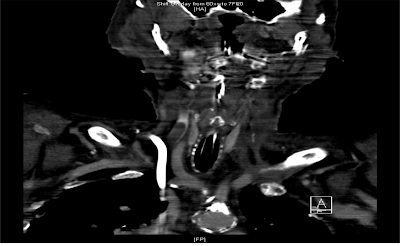
The following day she presented to the ED with dyspnea, tongue and facial swelling. A laryngoscope found laryngeal swelling and she was intubated emergently. She had a CT neck which is shown below:
(Click image for larger view)
She previously had received radiotherapy to her neck for a SCC of unknown origin which had left her with no jugular vein on the left and chronic supraglottic edema. Shortly after insertion of the line, a clot formed in her RIJ proximal to the catheter which, in the absence of a LIJ led to a SVC-like syndrome. She was treated with intravenous heparin and eventually removal of the catheter.
Catheter-associated thrombosis is surprisingly common. Prior to the 1990s the most popular route for inserting temporary dialysis catheters was the subclavian vein but this was increasingly recognized to be associated with subclavian thrombosis and stenosis. As a result, most lines are now inserted into either the jugular (preferable) or femoral veins. Up to 25% of patients with femoral lines develop associated thrombus which can be asymptomatic but may also present with signs of DVT or PE. But what about jugular lines? According to this study of 143 prevalent dialysis patients with RIJ tunneled dialysis catheters, 26% were found to have a catheter-associated thrombus while 62% of these had a complete occlusion of their RIJ. None of these were symptomatic.
So what can you do about this? In one way, ignorance is bliss. Given that they are usually asymptomatic, in the absence of catheter dysfunction, we should probably do nothing as if you removed every line simply because of the presence of an asymptomatic thrombus, you would run out of access site very quickly. Perhaps the lesson is this. In patients with previous surgery/radiotherapy to the neck or with multiple previous catheter insertions, determine the anatomy prior to inserting a new line so that any future complications can be anticipated and dealt with promptly.