A paper recently published in CJASN goes a long way towards answering these questions. This was a retrospective cohort study of all 1220 patients admitted to the ICU requiring CRRT in a single center in the Netherlands between 1994 and 2010. As expected, the in-hospital mortality was high (55%). Of those who survived, 12% did not recover enough renal function to come off dialysis after discharge.
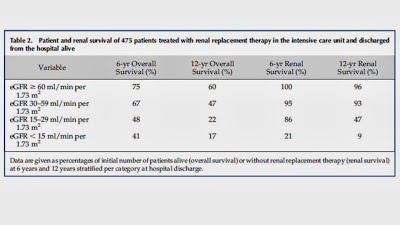
The commonest reasons for admission were thoracic surgery and sepsis. 20% of patients had pre-existing CKD, 48% had normal baseline renal function. There was no baseline in the remainder. At the time of discharge from hospital, 60% of patients had some degree of renal dysfunction (30% eGFR 30-60, 15% eGFR 15-30, 15% eGFR 0-15 including the 12% on HD). Of note, more than half of the patients with an eGFR <15 at discharge had pre-existing CKD. Unadjusted patient and renal survival is shown in the table:
The independent predictors of long term mortality were age, a surgical diagnosis, malignancy and an eGFR < 30. Similarly, the predictors of future need for dialysis were pre-existing CKD, and an eGFR < 30 at discharge. Interestingly, an eGFR between 30 and 60 was not associated with an increased risk of mortality or need for RRT in the future, relative to those with normal renal function at discharge.
This study adds to our knowledge of the predictors of outcomes after an episode of AKI requiring CRRT. No-one should be surprised that patients with significantly reduced GFR at discharge at are increased risk of mortality and need for eventual dialysis. However, it is reassuring that, in those patients who have an eGFR >60 at discharge, the likelihood of them requiring dialysis in the future is very low. It would be interesting to know if the presence of proteinuria modified the relationship between eGFR and mortality/need for dialysis, particularly in those with an eGFR between 30 and 60 at discharge but unfortunately, these data were not available.