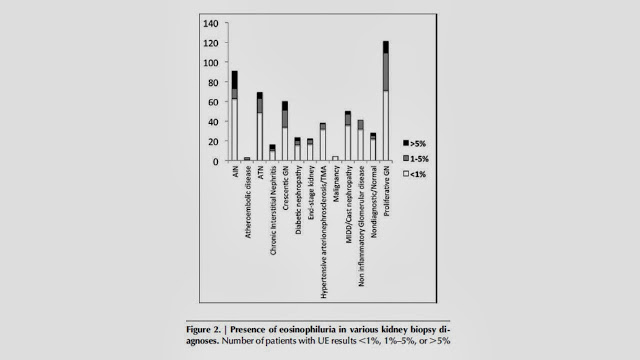
The authors examined the biopsy and urine results of 566 patients who had biopsies and a urinary eosinophil test over the course of the study. Overall 91 patients had biopsy-confirmed AIN, 73 of whom were considered to be drug-induced. 31.6% of patients had UE>1%, the traditional cut-off for the diagnosis of AIN. The majority of these did not have AIN and the distribution of positive UE was uniform across diagnoses. As a result, the sensitivity and specificity of this test for the diagnosis of AIN were poor. Using 1% UE as a cut-off, the sensitivity was 30.8% and the specificity was 68.2%. The PPV was 15.6% and the NPV was 83.7%. Using a more stringent cut-off of 5%, the sensitivity decreased to 19.8%, the specificity, PPV and NPV were 91.2%, 30% and 85.6% respectively.
One significant limitation of this study was that it was restricted to patients who had kidney biopsies and the majority of patients with suspected AIN do not have kidney biopsies. However, I would imagine that this should bias the results towards favoring UE as a test as presumably patients with more severe disease would be more likely to have a biopsy. Another issue is the potential that there was a bias towards biopsying patients who did not have UE (and so were not thought to have AIN in the initial impression). This could have the effect of reducing sensitivity.
Notwithstanding this, the fact that the distribution of positive UE was so well distributed among the various diagnoses combined with the very low sensitivity of this test would suggest that the use of this test should no longer be routine in the diagnosis of AKI. At best, a negative test helps rule out AIN in patients with a low pre-test probability while a positive test is not particularly useful. As the authors of the accompanying editorial point out, even in drug-induced AIN, the infiltrate may not have a high proportion of eosinophils, suggesting that in many cases there may not even be a plausible biologic rationale for this test.