PART 3: THE DANGERS
OF “DEPLETION”
OF “DEPLETION”
In my previous post concerning chronic severe hyponatremia,
I explained how over corrections of serum sodium of large magnitude required a
dilute large volume diuresis, often precipitated by resolution of a transient
source of ADH secretion. In this post I
will discuss two phenomena which are particularly dangerous as they carry
significant risk of producing large volume water diuresis.
I explained how over corrections of serum sodium of large magnitude required a
dilute large volume diuresis, often precipitated by resolution of a transient
source of ADH secretion. In this post I
will discuss two phenomena which are particularly dangerous as they carry
significant risk of producing large volume water diuresis.
1. Subclinical Volume Depletion: As
mentioned in my previous post, we noticed during our review of a large number
of cases of severe hyponatremia treated with 3% saline that most of the
patients whose serum sodium eventually overcorrected responded to small volumes
of 3% saline as if they were volume depleted, with sudden emergence of water
diuresis. Interestingly, most of these
patients were initially considered to be euvolemic by experienced
nephrologists.
mentioned in my previous post, we noticed during our review of a large number
of cases of severe hyponatremia treated with 3% saline that most of the
patients whose serum sodium eventually overcorrected responded to small volumes
of 3% saline as if they were volume depleted, with sudden emergence of water
diuresis. Interestingly, most of these
patients were initially considered to be euvolemic by experienced
nephrologists.
This very interesting paper reviewed the literature
concerning the value of physical examination in diagnosing volume
depletion. The conclusion, rather
humbling, was that other than in cases of severe volume depletion our physical
exam was quite inaccurate in diagnosing volume depletion. This is especially concerning considering
that establishing a patient’s volume
status forms the major decision point in the ubiquitous diagnostic algorithm
for hyponatremia.
concerning the value of physical examination in diagnosing volume
depletion. The conclusion, rather
humbling, was that other than in cases of severe volume depletion our physical
exam was quite inaccurate in diagnosing volume depletion. This is especially concerning considering
that establishing a patient’s volume
status forms the major decision point in the ubiquitous diagnostic algorithm
for hyponatremia.
According to the paper, reliable signs of volume depletion
usually are visible with the loss of about 20% of the intravascular
volume. The ADH secretion and response
to volume depletion starts with volume losses as low as 5-8% of the effective
intravascular volume. This implies that
the patient may have significant ADH secretion, contributing to the relative
excess water retention causing hyponatremia, while clinically appearing
euvolemic. It also means small volume
bolus may switch off this ADH secretion, causing water diuresis and sudden rise
in serum sodium.
usually are visible with the loss of about 20% of the intravascular
volume. The ADH secretion and response
to volume depletion starts with volume losses as low as 5-8% of the effective
intravascular volume. This implies that
the patient may have significant ADH secretion, contributing to the relative
excess water retention causing hyponatremia, while clinically appearing
euvolemic. It also means small volume
bolus may switch off this ADH secretion, causing water diuresis and sudden rise
in serum sodium.
Subclinical volume depletion as a contributor to
hyponatremia should always be considered a possibility especially when starting
therapy with 3% saline.
hyponatremia should always be considered a possibility especially when starting
therapy with 3% saline.
2. Solute Depletion Hyponatremia: The so
called “Tea and Toast Diet ” hyponatremia and “Beer
Potomania” are examples of solute depletion hyponatremia. As nicely described by Dr. Berl, our solute intake limits our ability to excrete free water. Even with a maximally dilute urine of around
50 mOsm/L, a person consuming a 300 mOsm/d diet can only excrete 6 L of urine
(300/50=6). Such a person will become
hyponatremic with drinking more than 6 L of fluids a day because any water in
excess of 6 L per day excretory capacity will be retained in the body. It is important to note that this water
retention is not due to ADH secretion.
ADH is often suppressed in such patients. The renal danger of this pathophysiological
mechanism is that whenever such patient is “presented” with solute
(IV normal saline, high-protein meal which would generate BUN or even 3%
saline!), without a high ADH level to prevent it, the added solute is used to
rapidly excrete free water that has been “trapped” in the body.
called “Tea and Toast Diet ” hyponatremia and “Beer
Potomania” are examples of solute depletion hyponatremia. As nicely described by Dr. Berl, our solute intake limits our ability to excrete free water. Even with a maximally dilute urine of around
50 mOsm/L, a person consuming a 300 mOsm/d diet can only excrete 6 L of urine
(300/50=6). Such a person will become
hyponatremic with drinking more than 6 L of fluids a day because any water in
excess of 6 L per day excretory capacity will be retained in the body. It is important to note that this water
retention is not due to ADH secretion.
ADH is often suppressed in such patients. The renal danger of this pathophysiological
mechanism is that whenever such patient is “presented” with solute
(IV normal saline, high-protein meal which would generate BUN or even 3%
saline!), without a high ADH level to prevent it, the added solute is used to
rapidly excrete free water that has been “trapped” in the body.
As an example, consider the case of the 26-year-old female
that I briefly alluded to in the previous post.
She presented with a serum sodium of 108 mEq/L after being on an
exclusively alcohol diet for the last 2 weeks.
She received 2 L of normal saline in the ER (154 mEq x2 = 308 mEq of
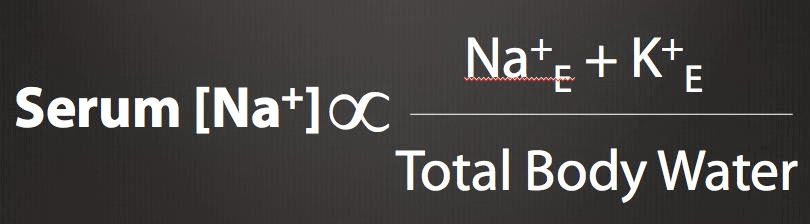
Na). Using the Edelman equation (see figure) and an initial total body water of
32 L, if we do not account for urine output, that amount of added NaCl would
have raised the serum sodium to about 111 mEq/L. But the actual rise of serum
sodium was to 131 mEq/L in about 5 hours accompanied by almost 7 liters of dilute
urine output. Her kidneys used the roughly 300 mEq of sodium in the NS bolus to
excrete more than 6 liters of maximally dilute urine (300/50=6 L, remember the
earlier calculation?) and almost perfectly accounts for the 23 mEq/L rise in
serum sodium (by reducing the denominator, TBW).
that I briefly alluded to in the previous post.
She presented with a serum sodium of 108 mEq/L after being on an
exclusively alcohol diet for the last 2 weeks.
She received 2 L of normal saline in the ER (154 mEq x2 = 308 mEq of
Na). Using the Edelman equation (see figure) and an initial total body water of
32 L, if we do not account for urine output, that amount of added NaCl would
have raised the serum sodium to about 111 mEq/L. But the actual rise of serum
sodium was to 131 mEq/L in about 5 hours accompanied by almost 7 liters of dilute
urine output. Her kidneys used the roughly 300 mEq of sodium in the NS bolus to
excrete more than 6 liters of maximally dilute urine (300/50=6 L, remember the
earlier calculation?) and almost perfectly accounts for the 23 mEq/L rise in
serum sodium (by reducing the denominator, TBW).
This would have also happened if she had received the same
amount of NaCl in the form of 3% saline as in such cases the volume of infusate
matters less than the amount of solute delivered.
amount of NaCl in the form of 3% saline as in such cases the volume of infusate
matters less than the amount of solute delivered.
I hope this case illustrates how dangerous solute depletion
hyponatremia can be and how easy it can be to precipitate an overcorrection of
serum sodium in such patients. This raises a very important question: if even
treatment with 3% saline is so unreliable in patients with chronic severe
solute depletion hyponatremia, how can we safely treat such patients? That will
be the subject of my next post.
hyponatremia can be and how easy it can be to precipitate an overcorrection of
serum sodium in such patients. This raises a very important question: if even
treatment with 3% saline is so unreliable in patients with chronic severe
solute depletion hyponatremia, how can we safely treat such patients? That will
be the subject of my next post.
In conclusion, subclinical volume depletion and solute
depletion pose a particularly tricky challenge in the management of chronic
hyponatremia as sudden rises in serum sodium level can happen rather easily in
these patients with, what would otherwise seem to be, rather innocuous
treatment with saline solutions.
depletion pose a particularly tricky challenge in the management of chronic
hyponatremia as sudden rises in serum sodium level can happen rather easily in
these patients with, what would otherwise seem to be, rather innocuous
treatment with saline solutions.
Posted by Hashim Mohmand


hiya, may i know what paper regarding about the clinical assessment of volume depletion? would like to have a good read
Great post about a really interesting topic!
One slight comment, though: Could you add the link to the paper mentioned (about the difficulty of assessing volume status)? That'll be great!