Monoclonal gammopathies generally arise from the development of
an abnormal clone of B-cell lineage. The monoclonal protein can be intact
immunoglogulin (often associated with free light chain), free light chain (FLC)
in isolation, or more rarely immunoglobulin heavy chain, either in isolation or
with associated free light chain. Monoclonal light chains have the ability
to self-aggregate and form tissue deposits either in the form of beta-pleated
fibrils (amyloid) or not (non-amyloid deposits).
an abnormal clone of B-cell lineage. The monoclonal protein can be intact
immunoglogulin (often associated with free light chain), free light chain (FLC)
in isolation, or more rarely immunoglobulin heavy chain, either in isolation or
with associated free light chain. Monoclonal light chains have the ability
to self-aggregate and form tissue deposits either in the form of beta-pleated
fibrils (amyloid) or not (non-amyloid deposits).
Monoclonal gammopathies may lead to kidney injury through a
variety of mechanisms, depending on the biochemical properties of the
light chain and/or immunoglobulin. These include: cast nephropathy (usually
kappa); monoclonal immunoglobulin deposition disease; crystal-storing tubulopathy;
amyloidosis (usually lambda), cryoglobulinemia or MPGN (membranoproliferative
glomerulonephritis).
variety of mechanisms, depending on the biochemical properties of the
light chain and/or immunoglobulin. These include: cast nephropathy (usually
kappa); monoclonal immunoglobulin deposition disease; crystal-storing tubulopathy;
amyloidosis (usually lambda), cryoglobulinemia or MPGN (membranoproliferative
glomerulonephritis).
Monoclonal gammopathies can frequently recur after transplant (Sethi et al. CJASN 2010). In a cohort of
transplant recipients in our center, Dr Batal had reported 8 cases of IgG/Kappa
MPGN, of which 3 failed post-transplant while 2 were still functioning; 3 were
lost on follow up (Batal et al. AJKD 2014).
transplant recipients in our center, Dr Batal had reported 8 cases of IgG/Kappa
MPGN, of which 3 failed post-transplant while 2 were still functioning; 3 were
lost on follow up (Batal et al. AJKD 2014).
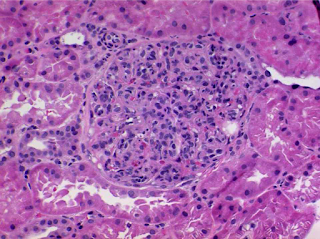
Recently, a 65 year-old Female with CKD secondary
to MPGN/IgG Kappa monoclonal gammopathy underwent a living-unrelated
kidney transplant. Creatinine came down to nadir of 1.2mg/dl three days after
transplant and then started to rise up to 2.5mg/dl. An emergent kidney biopsy
was performed which revealed aggressive MPGN (view picture above).
Immunofluorescence staining was negative for IgG, kappa or lambda. However, when
the biopsy sample was treated with pronase and restained, suddenly diffuse
Kappa staining was uncovered, confirming recurrence of her primary disease.
Pronase digestion has a denaturing effect on cell membranes, which may unveil
sequestered antigenic sites. This was previously shown to be useful in other forms of monoclonal
gammopathies such as in crystal-storing tubulopathy. Electron microscopy may also
help in identifying the deposits and triggering additional tests to elucidate
the composition of those. Unfortunately, prognosis of early recurrence is not
good and requires aggressive treatment against the possible source of light
chain (abnormal plasma cells) and removal of light chains from the circulation
through plasmapheresis.
to MPGN/IgG Kappa monoclonal gammopathy underwent a living-unrelated
kidney transplant. Creatinine came down to nadir of 1.2mg/dl three days after
transplant and then started to rise up to 2.5mg/dl. An emergent kidney biopsy
was performed which revealed aggressive MPGN (view picture above).
Immunofluorescence staining was negative for IgG, kappa or lambda. However, when
the biopsy sample was treated with pronase and restained, suddenly diffuse
Kappa staining was uncovered, confirming recurrence of her primary disease.
Pronase digestion has a denaturing effect on cell membranes, which may unveil
sequestered antigenic sites. This was previously shown to be useful in other forms of monoclonal
gammopathies such as in crystal-storing tubulopathy. Electron microscopy may also
help in identifying the deposits and triggering additional tests to elucidate
the composition of those. Unfortunately, prognosis of early recurrence is not
good and requires aggressive treatment against the possible source of light
chain (abnormal plasma cells) and removal of light chains from the circulation
through plasmapheresis.
To learn more about glomerular disease recurrence after
transplantation, refer to Kidney
Transplant iBook (Chapter 4/Section 8); Ponticelli et al. CJASN
2010; Ponticelli et al. CJASN
2011; and MPGN review on Sethi, Fervenza. NEJM
2012.
transplantation, refer to Kidney
Transplant iBook (Chapter 4/Section 8); Ponticelli et al. CJASN
2010; Ponticelli et al. CJASN
2011; and MPGN review on Sethi, Fervenza. NEJM
2012.