#NephMadness season is here! The #TransplantRegion has very interesting matchups, but one player that was left out of this contest because is relatively new in the game and relatively unknown, is Mesenchymal Stem Cells (MSCs). In the last few years the transplantation field has struggled to find how to prolong graft survival by inducing tolerance, minimize immunosuppression, inhibit fibrosis and treat rejection episodes. A candidate with all these characteristics are MSCs. MSCs are mesoderm-derived multipotent stromal cells that have high self-renewal and multi-lineage differentiation potential, anti-inflammatory properties, effects in the innate and adaptive immunity and the ability to repair damaged tissue.
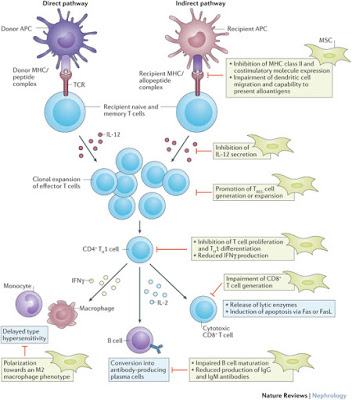
But what exactly makes MSCs attractive to transplantation? First of all, their effectiveness has been reported in the treatment of graft-versus-host-disease (GVHD). MSCs are found in fat, bone, cartilage, umbilical cord, cord blood, synovium, synovial fluid, muscle, skin and pulp and they can also be isolated from those organs, including the kidneys, which could be of major interest due to its repairing properties. MSCs inhibit T cell proliferation via several mechanisms including indoleamine 2,3 -dioxygenase (IDO) activity, production of prostaglandin E2 and transforming growth factor (TGF-β), expression of low levels of major histocompatibility complex (MHC) class II and costimulatory molecules including B7-1 (CD80), B7-2 (CD86) and CD40. They also inhibit macrophages, NK cell proliferation by reducing IFN-γ and dendritic cells (DCs) activity. In experiments, MSCs affect the ability of DCs to prime T cells in vivo. They also have direct effects on the endothelium by enhancing angiogenesis via expression of vascular endothelial growth factor (VEGF) and angiopoietins. The available data on B cells has not been studied extensively but some experiments report that MSCs increase CD4+, CD25+ and FoxP3+ regulatory T cell function (Treg) which may cause arrest of B lymphocytes in the Go-G1 phase of the cell cycle. In addition, MSCs by mediating T cells, inhibit the maturation, migration, proliferation and antibody production of B cells. Remember that FoxP3+ expression has an important role on Tregs. You can check details here in the #NephMadness Transplant Nephrology Science Region (#TransplantRegion). Although all these properties are exciting there are more questions than answers.
In mouse models of GVHD, MSCs were administered at 3, 8 or 20 days after bone marrow transplantation and other reports have suggested that a better immune suppression can be achieved when they are administered before transplantation, so clearly, there is no evidence for timing of administration. In regards to dosing and frequency, the MSCs proposed dose is 0.4 – 10 x 106 cells per kilogram of body weight in humans but using a high dose has also been reported. The frequency of administration has not been determined.
There are no reports on adverse events related to the infusion itself and long-term effects are not available, however in vitro and in vivo studies have shown that MSCs have the potential to differentiate into neoplastic cells and may promote growth of tumor cells.
In this report with autologous MSCs as induction therapy into living-related kidney transplant recipients, 159 patients were randomized to receive MSCs induction therapy with standard calcineurin inhibitor (CNI), MSCs induction with low-dose CNI or interleukin-2 (IL-2) receptor blocker. The authors reported reduced opportunistic infections in comparison to controls (HR, 0.42; 95% CI, 0.20-0.85; P = .02 ). Rejection episodes with MSCs induction were 8%, compared to 21% in the IL-2 receptor blocker group.
As of today (March, 2016), to my knowledge, there are 13 registered trials of MSCs in kidney transplantation that are currently recruiting patients or have been completed on the clinicaltrials.gov website. Other areas of interest in which MSCs are being used are acute kidney injury, chronic kidney disease and polycystic kidney disease. Most studies have used autologous MSCs since they seem to be more potent than allogeneic MSCs but it requires a long process and time can be an issue if recipients are in need of treatment for rejection. One advantage of allogeneic MSCs is that they can be available rapidly.
In conclusion, I think Tregs would have been a strong competitor in this year’s #NephMadness if MSCs would have qualified. Maybe next year or in the next few years they will be in better shape to compete in #NephMadness. MSCs may have a very important role in kidney transplantation given their immunosuppressive, reparative properties and potential to induce tolerance, however there are several technical aspects that are complex such as isolation, culture, amplification and cost, plus long-term outcomes are unclear at the moment and large clinical trials are needed.
Don’t forget to fill out your brackets!
Image from: Mesenchymal stromal cells in renal transplantation: opportunities and challenges. Nature, Feb 2016.