2016 marks the 7th year of the Top Nephrology Stories post on RFN. When this list first started in 2010 it was more challenging to get the stories. Now 7 years later, everything has changed. In my mind the advent of Twitter and NephJC has changed all of that. We are more informed and better read on nephrology topics. All you need to do is go over to NephJC and look at what is being talked about. Everything is there. Discussion is deep and constant.
Announcement:
- NephJC will host the #TopNephrology stories starting in 2017.
- We will use analytics from each of the chats throughout the year plus feedback from the NephJC team to create a #TopNephrology list.
We hope these changes will result in an improvement and reflect the Top 10 stories that you need to be aware of. RFN is not going away and we have big plans for RFN. If you are a fellow and interested in posting to RFN please send me an email or DM.
Below are links to the last 6 years of the top nephrology stories hosted on RFN.
10. HLA-incompatible live kidney donation survival benefit in NEJM (5%)- Coming in as a tie for number 10 is a study reported in NEJM (March 2016) and covered by NephJC. It is well known that kidney transplantation is the best form of renal replacement therapy. However, there is a limited number of organs to meet the growing demand. Furthermore, patient related factors such as the presence of anti-HLA antibodies are another factor lengthening the wait time and often preventing transplantation. This study looked at matched patients (not a randomized trial).
- One group of kidney transplant recipients undergoing a desensitization protocol with a live donor incompatible kidney transplant
versus
- A matched group who underwent deceased donor kidney transplant with a match or remained on the wait-list.
The study looked at multiple kidney transplant centers between ’97-’11 The results were striking. Patients who underwent a live incompatible kidney transplant with desensitization protocol had a significant survival advantage compared to wait-listed patients and wait-listed + deceased donor. However, it must be noted that the desensitization protocol itself has side effects and careful consideration is needed before using this method. This study is important because it represents a significant advance in generalizing the use of desensitization for patients unable to obtain a kidney transplant because of preformed antibodies.
10. ELAIN Trial of early versus late HD in the ICU in JAMA (5%)- This spring started off with a bang. Back to back presentations of renal replacement therapy in the ICU showing different results. First the AKIKI Trial (our number 3 story) was presented at the Critical Care meeting in San Diego and reported in NEJM and showed no difference in early versus late. A few weeks later came the ELAIN (Early vs Late Initiation of Renal Replacement Therapy in Critically Ill Patients With Acute Kidney Injury) Trial. This was a single-center randomized trial presented at the ERA-EDTA Congress in Vienna, and reported in JAMA. They found a significant reduction in 90-day all-cause mortality in the early initiation group. Some important caveats.
- This was a single center study (AKIKI was multicenter).
- Majority of patients were surgical ~80% (AKIKI ~80% medical)
- 100% were CVVHDF (AKIKI ~30% CRT)
- Only 4% in late group avoided RRT (~50% in AKIKI).
Bottom line- these were very different studies and hence had very different results. Could a select group of patients with a more defined ischemic insult benefit from early RRT in the ICU? Jury is still out but the ELAIN Trial would suggest this to be true.
9. EuLite Trial of high cutoff dialysis in myeloma presented at UK Kidney Week (6%)- The long awaited results from the EuLite Trial were presented at UK Kidney Week this year. See Paul Phelan’s post on RFN from way back in 2013. Unfortunately, the EuLite Trial isn’t published just yet so we have is the live Twitter coverage from the meeting. The premise is that High Cutoff (HCO) Dialysis would provide benefit from removing toxic free light chains in myeloma cast nephropathy. HCO dialyzers employ high flux membranes with particularly large pores (up to 50kDa Vs 15kDa for conventional high flux) facilitating the removal of large plasma proteins such as FLC (kappa and lambda light chains have molecular weights of 22kD and 45kD respectively). The EuLite Trial is a randomized clinical trial testing the use of HCO dialysis versus standard dialysis in patients with myeloma case nephropathy. Unfortunately, HCO Dialysis arm of the study had more mortality compared to the standard HD arm hinting at harm. We all eagerly await the full publication to be reported to we can really delve deep into this study. Looks like the early enthusiasm for HCO dialysis in myeloma cast nephropathy is fading as well.
7. Contrast nephropathy study in JASN (8%)- September brought a bombshell of a study. The Wilhelm-Leen, Montez-Rath and Chertow paper looked at the risk of acute kidney injury in the days following a dose of radiocontrast. And the researchers could find no hint of AKI. To say this counters nephrology dogma is an understatement. If Moses had brought down the Nephrology Ten Commandments, Thou shalt avoid radiocontrast would probably be in the top three, following only by Thou shalt monitor and control one’s blood pressure and Thou shalt not eat so much salt. The investigators used NIS, the largest publicly available all-payer inpatient care database, this covers 96% of the US population and used diagnosis and procedure codes to find exposures and acute kidney injury. Despite that limitation the result is so provocative that it begs relooking at this toxicity with open eyes. Of note similar findings have been published in the radiology literature for years: McDonald JS, Bruce RJ, while others have upheld the orthodoxy.
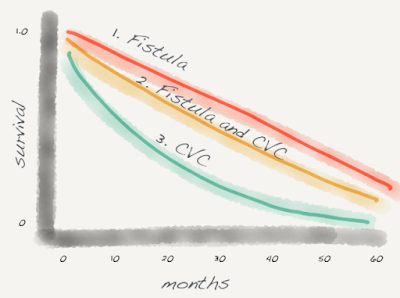
7. “Fistula First” survival benefit is due to patient factors in JASN (8%)- If contrast nephropathy is really just a figment of confirmation bias, then at least we know that fistulas are the best hemodialysis access and convey a true survival benefit. Or maybe we don’t know that. The same issue of JASN brought us the work of Robert Brown, Bhanu Patibandla and Alexander Goldfarb-Rumyantzev. The thread that triggered this investigation was the repeated observation that every study that revealed a survival benefit for starting with a fistula (all observational and retrospective data) also showed that catheter patients were different from patients starting with a fistula. Often the catheter patients were older, more urban, shorter pre-ESRD nephrology care, more diabetes, more cerebrovascular disease, and more heart failure that the patients starting with a fistula. The authors looked for a way they could separate fistula patients from these inherent biases that could explain the survival benefit these patients enjoyed. The authors divided elderly new starts to hemodialysis into three groups:
- Started dialysis with a fistula
- Started dialysis with a central venous catheter, but had a fistula that was maturing when they started dialysis
- Started dialysis with a central venous catheter
If the fistula was driving mortality, group 2, that is dialyzed with a catheter, should have outcomes similar to group 3. If the patient characteristics were driving the survival advantage of the fistula, group 2 should look like group 1.
The money quote from the conclusion
although this study has confirmed the approximately 50% decreased mortality experienced by patients initiating hemodialysis with an AVF compared with a catheter, it showed that about two thirds or more of this mortality benefit is also seen in those initiating hemodialysis with a catheter but who had previously undergone unsuccessful fistula placement. Thus, these observational data suggest that the actual mortality attributed to the catheter itself is much less than previously considered and may be explained in large part by differences in patient factors.
Similar conclusions were published in JASN this October using Canadian data. That team is planning on confirming these results with a randomized controlled trial of fistulas versus catheters (see this Medscape article, log in required). That will be amazing!
6. US Congress expands Medicare coverage for acute dialysis coverage (10%)->In June of 2015 the nephrology world suddenly became very interested in the Trade Preferences Extension Act of 2015. Because politics is hard, an important bill for acute kidney injury got stapled to this larger “Transporter bill”. On June 29th President Obama signed the bill and section 808 became law.
Specifically, Section 808 of the law amends the Medicare statutes to provide coverage for “renal dialysis services furnished … by a renal dialysis facility or provider … to an individual with acute kidney injury.”
This overturned a CMS ruling from 2012 that forbid medicare reimbursement to dialysis providers for the condition of acute kidney injury. This left lots of patients in a lurch. Patients unfortunate enough to develop AKI often would recover from their acute illness but they would have to remain in, or close to, the hospital as their acutely dtysfunctioning kidneys recovered or didn’t. Until a nephrologist was willing to give up hope and declare the patient ESRD, that patient would not be able to receive dialysis anywhere but the hospital. This esoteric bureaucratic red tape of where and when people could get dialysis hurt patients and it is nice to see this straightened out, even if it was passed in 2015 and doesn’t go into effect until January 1, 2017.
5. Nephrology societies embrace social media (11%)- Most of the nephrology societies have had a social media presence for many years (see this Twitter list from Joel Topf) however, 2016 marked some sort of a watershed in the seriousness, enthusiasm and effort taken by many of them to really engage with social media.
The American Society of Nephrology (ASN) has a very active Twitter presence, and actively tweets out the latest breakthroughs in research and other news in the nephrology universe. Along with ASN Kidney News and ASN Advocacy, the two flagship journals, JASN and CJASN, also have active Twitter handles, and are progressively using the medium effectively for communication. But two other initiatives stand out in all the things the ASN does on social media this past year: #askASN and ASN communities. Once every month, the ASN brings forward an expert for the #askASN chats (some of the featured guests include Richard Lafayette who runs Kidney News, POTASN Ray Harris and PEOTASN Eleanor Lederer, KidneyWk organizers Roy Zent and Patrick Nachman, and SPRINT investigators George Bakris and Bill Cushman) to answer questions from the nephrology Twitterverse. Secondly, a few months ago, spearheaded by Zachary Cahill, the ASN launched a forum, ASN Communities. It has gathered steam, and now boasts 8 separate communities (the Open Forum and Patient Care being most active, with Onconephrology, Transplant, AKI, Basic Science, Supportive Care, Training Program Directors being the others), with over 3,000 discussion threads!
The ERA-EDTA has been on Twitter for a while, but they publish two journals, and until recently didn’t have a social media presence. But they stepped nicely to a request, and @NDTsocial and @CKJsocial were born. Both have been actively tweeting out snippets of the latest nephrology literature (with CKJ continuing to be an #openaccess journal) over the last year.
The International Society of Nephrology (ISN) is ramping for the upcoming World Congress of Nephrology, scheduled to be held in Mexico in 2017. The ISN does have an active education committee and holds regular webinars, but for the WCN, they have established a WCN 2017 social media task force make up of 20 nephtweeters from around the world. We look forward to their coverage of the WCN2017. Now only if someone could persuade Kidney International to join Twitter…
The National Kidney Foundation (@NKF) is also active on Twitter and actually sets the record for number of followers ~19,000. The NKF Spring Clinical Meeting (@NKFClinicals) was much more active this year and featured a live social media workshop. Next years meeting is featuring a social media ambassadors program at SCM17. Of course AJKD was an early adopter of social media and a leader in the space with AJKD blog, NephMadess, and AJKDonline Twitter handle.
4. Empagliflozin approved for CV indication by FDA (13%)- A common refrain in the diabetes literature has always been a lack of benefit seen for hard outcomes with hypoglycemic agents, with metformin being a lone exception. This all changed with the EMPA-REG trial, which made it to the #TopNephrology stories in 2015 as number 2. At that time, we just had the late breaking trial to work on, but it was already huge news. The subsequent publication in NEJM was covered at a #NephJC session too. The need for this trial to be done is very interesting – until recently, showing a drug lowers blood sugar was the most important aspect of getting FDA approval. After the debacle behind rosiglitazone (avandia) and the possible risk of greater cardiovascular events despite lower blood sugar, the FDA mandated larger trials to demonstrate CV safety. EMPA-REG was one such trial, and demonstrated remarkable benefit in lowering CV outcomes. The FDA followed suit, and on Dec 2 announced a new indication for empaglifozin – for reducing cardiovascular death in patients with type 2 diabetes. The SGLT-2 inhibitors have indeed come a long way in a short period of time.
3. AKIKI Trial of early versus late dialysis in the ICU in NEJM (20%)- Coming in at #3 in this years poll is AKIKI. AKIKI was also the winner of the #NephJCKidneys at KidneyWk for Study of the Year. The timing of renal replacement therapy has been rated as a top priority for research in the AKI world. Indeed, in the last few years, clinical practice has slowly crept ahead of evidence, as it often does, and dialysis is being initiated earlier and earlier for acute kidney injury. And then came along the Artificial Kidney Initiation in Kidney Injury (AKIKI) trial, to do what IDEAL did for timing in the chronic dialysis field. In this trial, 620 patients with AKI were randomized to either early strategy (with RRT initiation at stage 3 AKI per KDIGO criteria) or delayed strategy, when a clinical indication occurred (eg hyperkalemia, pulmonary edema, or persistent oliguria > 72 hours). There was no difference in mortality, with only half the patients needing dialysis in the delayed group, who also had significantly less bloodstream infections. Check out the #NephJC coverage for more details.
2. PPI and CKD risk in JAMA Internal Medicine and JASN (22%)- This was big. Another important paper dropped in nephrology literature during springtime. We had AKIKI, ELAIN and now PPI causing CKD all Feb to April. The PPI leading to CKD story was first reported in JAMA Internal Medicine then in JASN. NephJC covered this and you can view the background and both chats here. While a rare association between PPI use and interstitial nephritis has been known for a while. Their association with chronic kidney disease had not been reported before. The JAMA Internal Medicine paper is an observational, prospective cohort study with two cohorts. The first is the Atherosclerosis Risk in Communities (ARIC) study, of which 10,482 participants were included. The second was the much larger Geisinger Health System Replication (GHSR) Cohort, with 248,751 participants. Participants using either PPIs or H2 antagonists were compared with each other to evaluate their respective risk of developing kidney disease.
A propensity score-matched analysis was conducted to minimize confounding variables and identify whether baseline PPI use was associated with CKD. It is important to note that PPI users in both cohorts were more likely to have a high BMI, hypertension, cardiovascular disease, and exhibit polypharmacy (with antihypertensives, aspirin, diuretics and statins). They found that PPI use is associated with a higher risk of incident CKD. The JASN paper from Xie et al used a Department of Veterans Affairs national databases to build a primary cohort of new users of PPIs (173,321) and new users of H2 blockers (20,270) and followed these patients over 5 years to ascertain renal outcomes. In adjusted Cox survival models, the PPI group, compared with the H2 blockers group, had an increased risk of incident eGFR decline less than 60, incident CKD, and a graded association between PPI duration and risk of renal outcomes. Both of these studies point to a fundamental issue in medicine. Polypharmacy. We need to remain vigilant to remove medication that have no clear indication. PPIs once thought of as innocuous now have real risk associated with them.
1. suPAR from bone marrow myeloid cells in Nature Medicine (64%)- Coming in at # 1 this year is a basic science paper just published a few weeks ago in Nature Medicine. Just like the Gli1 story of 2014 we will also have to add an asterisks to this win. The suPAR aficionados really came out in force with heavy voting and it is not a surprise for us as suPAR has been a consistent story for the last 7 years. suPAR graced the TopNephrology stories in 2011. In fact, it hit the number 1 spot with the original Nature Medicine paper describing its potential link to FSGS. Then in 2015 suPAR was unable to crack the top 10 and landed at number 14 with the NEJM paper linking suPAR to CKD in a cohort of patients at Emory undergoing cardiac catheterization. Now in 2016, suPAR does it again. Our #1 story. The current study seeks to identify with cellular source of soluble urokinase plasminogen activator receptor (suPAR) which the above studies have implicated in CKD. Most notable is the fact that if a patient with FSGS receives a kidney transplant unfortunately their is a high chance of recurrence. Thus, implicating an extra renal “factor” like suPAR leading to kidney damage. Utilizing a combination of bone marrow chimera, ablation and cell transfer studies that suggest that Gr-1lo immature myeloid cells of bone marrow origin is the source of suPAR and a key contributor to glomerular damage. A very interesting observation that will no doubt lead to more studies on the link between bone marrow derived cells and kidney function.
Another busy and exciting year in the world of nephrology in 2016.
Thanks to all of the contributors and readers in the nephrology online
community for keeping nephrology fun, interesting and educational. Next year the #TopNephrology stories will be moving to NephJC.
Thanks for supporting RFN and NephJC. Happy holidays from the entire team.
Can’t wait to see what 2017 has in store!
Don’t forget to sign up for the NephJC email to keep up to date
Post by Matt Sparks, Swapnil Hiremath, and Joel Topf


12. HLA-incompatible live kidney donation survival benefit in NEJM (5%)
13. 5-year on-pump/off-pump CABG kidney failure rates similar CORONARY Trial in NEJM (4%)
14. Oxalobacter formigenes stimulate oxalate transport by the gut in JASN (3%)
14. Facebook app to increase kidney donation in Am J Transplant (3%)
16. Fatty acid oxidation in tubular cells important for kidney fibrosis in Nature Medicine (2%)
17. Blood pressure regulation by CD4+ T cells expressing choline acetyltransferase in Science Signaling (1%)
Excellent
Excellent synopsis. Thank you for your continued hard work and service to the Nephrology community.
@Nephro_Doc