 |
| Figure 1 |
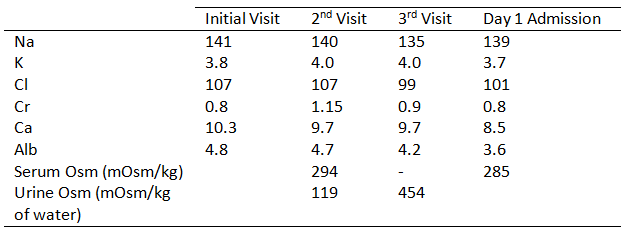
Ms. Phursty is a 66 year old Caucasian woman with a past medical history of Graves’ disease who was referred to nephrology for polydipsia. She endorsed extreme thirst for the last 3-4 months drinking 6 glasses of 32 oz water daily. She craved water only and did not consume other liquids such as tea, coffee, juice, or alcohol. She denied any nocturia or dysuria. There had been no changes in medications or other habits. She reported no NSAID intake or any herbal supplements. Her demeanor was very concerned and reported she was afraid to leave home for too long with an insatiable need to drink and urinate. Vitals were not remarkable. The physical exam revealed a thin, middle-aged woman sitting comfortably. She had a normal neck exam without goiter, no abnormalities in chest or abdominal exam, and was without rash or edema. Initial labs are available in Table 1, with a normal liver panel, normal glucose, and HgbA1c 5.8. Her urinalysis showed SG 1.003, and was negative for glucose, bilirubin, protein, ketones and blood. Given her concern for thirst and very dilute urine, there was clinical concern for diabetes Insipidus (DI). Urine osmolarity and electrolytes were ordered and follow up was scheduled one week later.
 |
|
Table 1. Labs from outpatient clinic and initial admission
|
The patient returned with continued polydipsia and polyuria, and repeat labs in Table 1. Her PTH was 80 pg/mL (high) and Vitamin D 25-OH 17 ng/mL (low). Urine osmolarity was 119 mOsm/kg, UCr 26, UNa 16, UK 6 and UCl less than 20 (all units mEq/L). Serum osmolarity was elevated to 294 mOsm/kg. A subsequent inpatient 24-hour urine collection revealed a volume 1.9L, CrCl 100 mL/min, UNa 34 mmol/d, UCl 27 mmol/d, UUrea 8 g/d, Uosm 287 mOsm/kg of water, and total urine osmoles 545. Her urine output was much lower than expected and very dilute with low solute intake. A 4-hour water restriction test began and was followed by DDAVP 2 mcg IV with results in Table 2.
 |
|
Table 2. Serum and
Urine osmolarities during the water restriction test with DDAVP |
Final results of the water restriction test and administration of DDAVP revealed normal response with increased urine osmolarity to appropriate high levels. This ruled out a Central Diabetes Insipidus (CDI) and Nephrogenic Diabetes Insipidus (NDI) respectively. Osmotic Diuresis was excluded as her urine osmolarity was below the serum osmolarity over 24 hours, and she had appropriate solute in the 24-hour urine collection. The patient had a final diagnosis of primary polydipsia when water restriction testing demonstrated a Urine Osm greater than 500 mOsm/kg of water. The findings were discussed and counseled that she would need behavior modification and professional guidance to control her excessive thirst.
Primary polydipsia, (PP, formerly called Psychogenic Polydipsia), is usually seen in middle-aged women and is common in those with psychiatric disorders.
- Hypothalamic disorders have been reported to alter the thirst regulation center and systemic infiltrative disorders such as sarcoidosis can lead to this.
- A large number of medications can lead to dry mouth and thirst and must be ruled out as a cause prior to PP diagnosis.
- Differentiating PP from CDI and NDI is paramount on the urine studies.
- Central Diabetes Insipidus is lack of partial or complete ADH production.
- Nephrogenic Diabetes Insipidus is a lack of response to adequate ADH release in the setting of a rising serum osmolarity above normal 285 mOsm/kg.
- Nephrogenic Diabetes Insipidus can be caused from electrolyte derangements such as hyperglycemia, hypokalemia, and hypercalcemia inducing a poor response of the nephron to antidiuretic hormone.
 |
| Figure 2 |
Workup of a patient with polyuria must be carefully performed with accurate timing and measurements of oral intake, urine outputs, and electrolytes. A 24-hour urine collection study will reveal solute output and help determine if increased solute intake is driving diuresis Figure 1. If a patient has a normal sodium of less than 145 mEq/L, a water restriction test should be performed for 4 hours. This will cause a slow rise in serum osmolarity, with subsequent release of ADH. The presence of ADH should lead to urine osmolarity changes depicted in Figure 2. After 4 hours, DDAVP should be given to supply appropriate levels of ADH and to monitor urine volume and urine osmolarity. Final response to water restriction and DDAVP administration is shown in Figure 3.
 |
|
Figure 3. Sands JM, Bichet DG. Nephrogenic Diabetes
Insipidus. Ann Intern Med 2006;144:186-194. |
A polyuric and/or polydipsic patient is a not uncommon outpatient consult for a Nephrologist. Carefully collected history and data are critical to flushing out the correct diagnosis.
**This is a fictional case of a thirsty Ms. Phursty.
Gates Colbert, MD
Kidney and Hypertension Associates of Dallas
Clinical Assistant Professor, Texas A&M College of Medicine
Baylor University Medical Center at Dallas
NSMC Intern Class of 2017
