What is the Fistula First Initiative?
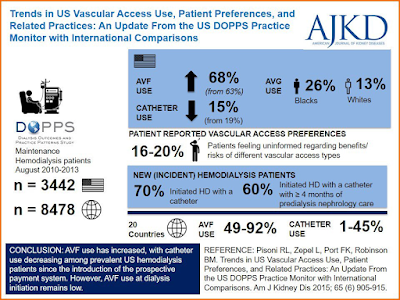
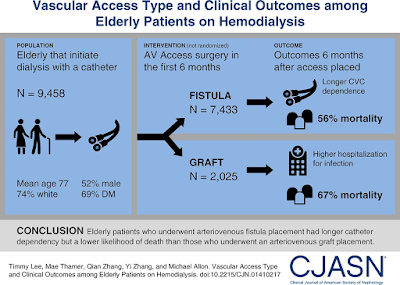
The Fistula First Initiative (FFI) is a national quality improvement project that was established in 2003 to increase the use of arteriovenous fistula (AVF) for hemodialysis (HD) access in incident and prevalent patients. The aim of FFI was to have a functioning AVF in 66% of the prevalent dialysis population. The use of central venous catheters (CVC) before FFI was quite high and was significantly associated with increased morbidity and mortality mainly due to catheter related blood stream infections as well as increased costs due to hospitalizations and other complications. A recent DOPPS report shows an improvement in AVF use among prevalent patients in the US, however 70% of incident HD patients still started with a CVC (See #VisualAbstract below).
What are the advantages and disadvantages of AVF?
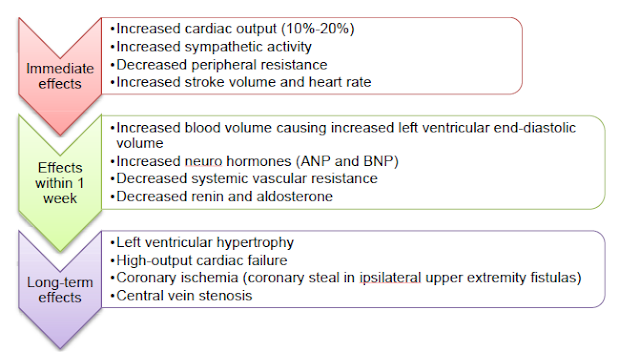
AVF was promoted as the best hemodialysis VA due to its superior patency, low complication rate (especially infection and thrombosis) and low overall cost. However, creating a functional AVF is sometimes not that simple and straightforward. It turns out that creating an AVF is not the only challenge, rather, the major hurdle limiting it is maintaining its patency. As the rate of AVF creations increased, the rate of primary failure increased as well, along with an increase in the use of central venous catheters (CVC) as a bridge for a maturing AV access. Factors contributing to fistula failure of maturation include; advanced age, female gender, diabetes, coronary artery disease (CAD) and peripheral vascular disease (PVD). Furthermore, the hemodynamic changes after AVF creation (see figure) can be of serious concern, particularly in patients with pre-existing cardiovascular diseases for e.g. in patients with heart failure, where a successful AVF may actually worsen the underlying heart failure.
Vascular access in elderly:
Vascular access placement in the elderly is a prime example of why the FFI may not always be ideal. There are several reasons for this conundrum:
1. Timing of access placement.
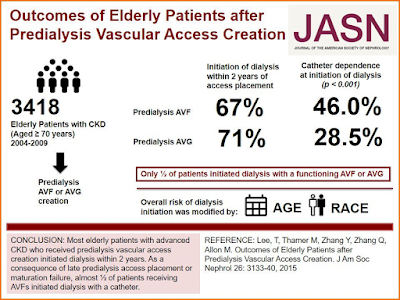
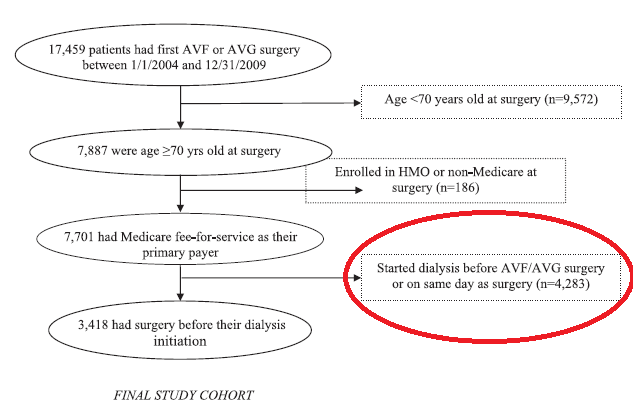
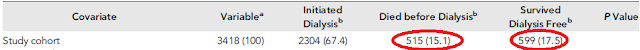
In a study published in JASN, 4283 elderly patients (out of 7701) initiated dialysis before AVF/AVG placement or at the day of surgery and were excluded from the study.
Also, 15% of included patients died before dialysis, and 17.5% did not need dialysis until the end of the study (denoting early VA placement). This makes predicting the optimal time for AVF creation more challenging.
2. Shorter survival of elderly patients with multiple comorbidities makes it more likely that these patients may die without ever requiring dialysis (as shown in the table above).
3. High rate of maturation failure
This remains one of the biggest challenges to increase the use of AVF, more so in the elderly.
In the same study, 50% of elderly patients with an AVF, actually initiated dialysis via a CVC due to failure of maturation of the AVF. In contrast, only 28% of those with a predialysis AVG needed a CVC at start. Thus, Lee and his group suggested more liberal use of AVG for elderly CKD patients approaching dialysis. They concluded that an AVG creation, closer to dialysis initiation, may serve as a “catheter-sparing” approach.
The Unclear case for AVG
An AVG has 2 main advantages: shorter time to cannulation and the less frequent need for interventions. This is supported by earlier findings that creation of AVF in elderly patients with CKD (6–9months) was not associated with better AVF success at dialysis initiation, but resulted in more predialysis interventional access procedures. Another important finding was that in patients with CKD aged greater than 80 years, predialysis AVF creation demonstrated no clear survival benefit compared with AVG creation.
However, the hypothesis that, AVG placement after dialysis initiation with a CVC will result in shorter CVC dependence and lower infections and mortality, was not supported by retrospective observational data. Instead, they observed that elderly patients initiating hemodialysis with a CVC undergoing an AVF placement within 6 months had fewer hospitalizations due to infections and a lower likelihood of death than those receiving an AVG, despite extended CVC dependence in the AVF group. (See #VisualAbstract below).
In conclusion, in the era of precision medicine and individualized care, one size doesn’t fit all and fistula may not always be First! Elderly patients have high rate of primary access failure, which increase CVC use as a bridge for another access or AVG. Studies are needed to figure out how to predict which patient will have primary failure of maturation, so as we can plan for better management of his vascular access.
Mohamed Elrggal
Nephrologist
Alexandria, Egypt
NSMC Intern, Class of 2018



2 comments