One of my mentors, Dr. Fred Silva, frequently reminds us that
“the kidney has a limited number of ways to respond to an innumerable number of injuries”.
For this reason, studying kidney pathology is challenging and fun. Since the same pattern on light microscopy can be seen in several disease states, it’s the combination of the morphology, immunofluorescence, and electron microscopic findings in the context of a clinical history and laboratory testing that allows us to give the best possible and most robust diagnosis. When all of these components align the pathologist can help the nephrologist distill the pattern of pathologic findings to a single etiology for the patient’s presentation in a majority of cases.
When pathologists receive biopsies with limited history, clinicopathologic correlation can be extremely challenging. This is especially important in renal pathology, where “. . . proper kidney biopsy interpretation usually requires significant clinical knowledge” (Truong & Herrera, 2009), compared to general surgical pathology, where a diagnosis cannot be made without history in less than one percent of cases (Nakhleh et al, 1999). To emphasize how critical the clinical context is to the nephropathologist, here are some examples
Context is key– Consider a kidney biopsy where the only history received is a “37 year old female”. The biopsy shows endocapillary proliferative lesions on light microscopy, IgA and C3 positivity by immunofluorescence, and mesangial and paramesangial electron dense deposits on electron microscopy. The pattern could fit with an active IgA nephropathy. Consider then that the patient has a history of Intravenous drug use with a known Staphylococcus aureus bacteremia. The clinical context makes a diagnosis of infection-associated glomerulonephritis far more likely. This context not only affects the diagnosis, but also the management of the patient. In the first clinical scenario treatment with steroids may be required, however, in the second scenario, antibiotic therapy and treatment of the underlying infection is required and steroid treatment may adversely affect the outcome. It’s ultimately the context that provides the diagnosis and directs an optimal therapy for the patient.
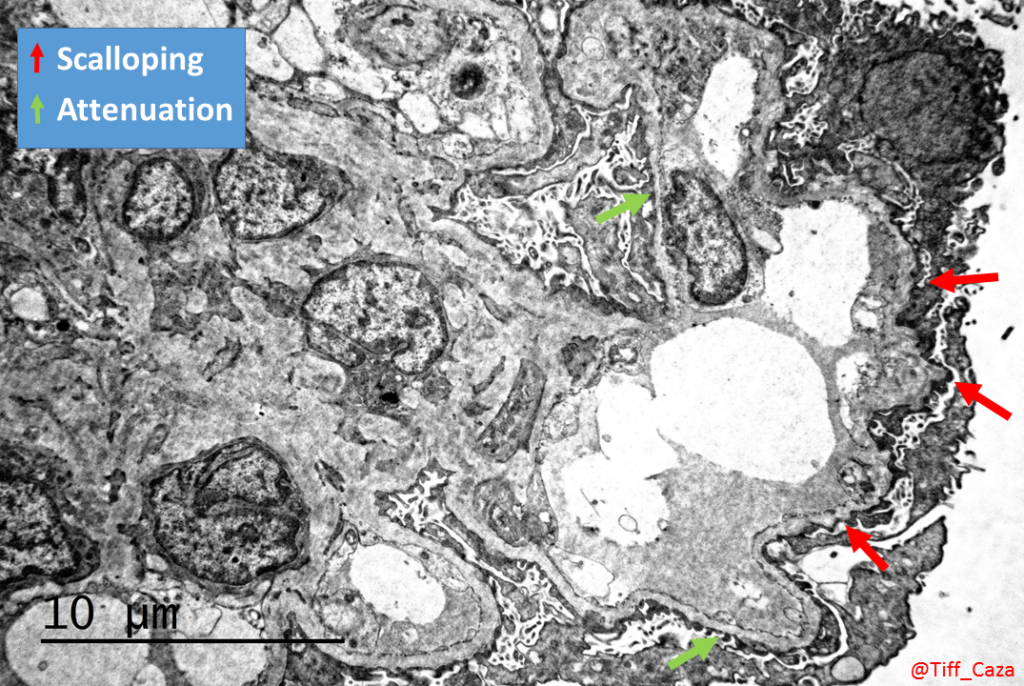
Again, context is key- Here’s another example, with a history of a “28 year old male”. The biopsy shows no significant findings by light microscopy, a negative immunofluorescence, and glomerular basement membrane abnormalities with scalloping and early lamination on electron microscopy. These results could be concerning for type IV collagen abnormalities and trigger a workup for Alport syndrome (Kashtan et al, 2018). However, on review of clinical information it emerges that the patient had presented with membranous glomerulopathy at age 25, was treated, and has low level proteinuria thereafter. The glomerular basement membrane abnormalities could be interpreted as remodeling changes from resorbed immune deposits. The context assists the diagnosis. In this case, there is likely less of an impact on patient care, but there may be increased health care costs due to unnecessary testing
Clinical clues trigger additional studies- Clinical findings may also trigger us to “dig deeper” to look for diagnostic changes. Consider a rare red blood cell cast is identified in a case with diabetic nephropathy. Microaneurysms can occur within diabetic glomeruli and result in microscopic hematuria and rare red blood cell casts. This would unlikely to trigger additional workup. However, if the patient had a history of a positive ANCA serology, this may trigger the pathologist to do several additional levels to examine for a necrotizing or crescentic lesion. Focal findings can be missed due to sampling if the disease process of interest is not on our radar.
Native or transplant matters– The opposite can also occur, where pathologic findings can be overcalled without history. Consider a case being worked up as a native biopsy, yet was a transplant. If the biopsy shows endocapillary hypercellularity within glomeruli with global glomerular capillary loop double contouring, it could be diagnosed as a membranoproliferative glomerulonephritis, when in fact, this could represent chronic active antibody mediated rejection in the context of a transplant.
We can avoid these misinterpretations by obtaining adequate and focused history with the biopsy. Taking 5 minutes to provide some information to the pathologist can save more time in the future, will provide a better diagnosis, and lead to optimal patient care.
These are the elements that are most useful to your pathologist:
- Age and ethnicity
- Indication for biopsy, such as acute kidney injury, nephritic syndrome, nephrotic syndrome, chronic kidney disease, isolated hematuria, or transplant
- Medical comorbidities
- Family history of kidney disease
- Medications
- Metabolic panel and a baseline serum creatinine
- Serologies: ANA, ANCA, Hepatitis B, Hepatitis C, HIV
- Serum protein electrophoresis, urine protein electrophoresis, or serum free light chain assay
- Urinalysis
Here’s an example of a five minute history that can be provided to the pathologist with your biopsy: “The patient is a 44 year old African American man who presents with worsening CKD. Co-morbidities include hypertension. There is a family history of ESKD in the mother and CKD in a sister. Medications include lisinopril and amlodipine. BUN is 30 mg/dL, creatinine is 2.5 mg/dL (baseline 1.0 mg/dL 4 years ago), and albumin is 3.5 mg/dL Serologies (ANA, ANCA, HIV, Hep B, Hep C) are all negative. SPEP is negative for a paraprotein. UA shows hyaline casts and 3+ proteinuria, quantified by UP/Cr at 2.7 g/g.”
Let’s say the biopsy showed global and segmental glomerulosclerosis with moderate tubulointerstitial and vascular scarring, negative immunofluorescence, and moderate podocyte foot process effacement by electron microscopy. While these changes can be attributed to chronic injury due to arterionephrosclerosis, in this clinical context, there is suspicion for APOL1-associated disease.
As an alternative, you could simply print out a progress note and a set of labs. This will provide most or all of the above information. Clinicopathologic correlation can continue after the biopsy read by discussing the results with the pathologist, and we can learn from one another. Together, the nephrologist and pathologist can create a powerful team to provide a right diagnosis for the patient and provide optimal patient care.
Tiffany Caza MD/PhD @Tiff_Caza
Nephropathology Fellow
NSMC intern 2019
*All cases depicted above are hypothetical cases and do not represent real patient cases.


