In 1996, the Institute of Medicine defined telemedicine as the use of electronic information and communication technologies to provide and support health care when distance separates “participants”. Telehealth is a broad term encompassing the use of electronic communication to provide clinical care and includes interactive videoconferencing, remote monitoring, e-mails etc. (Fig 1).
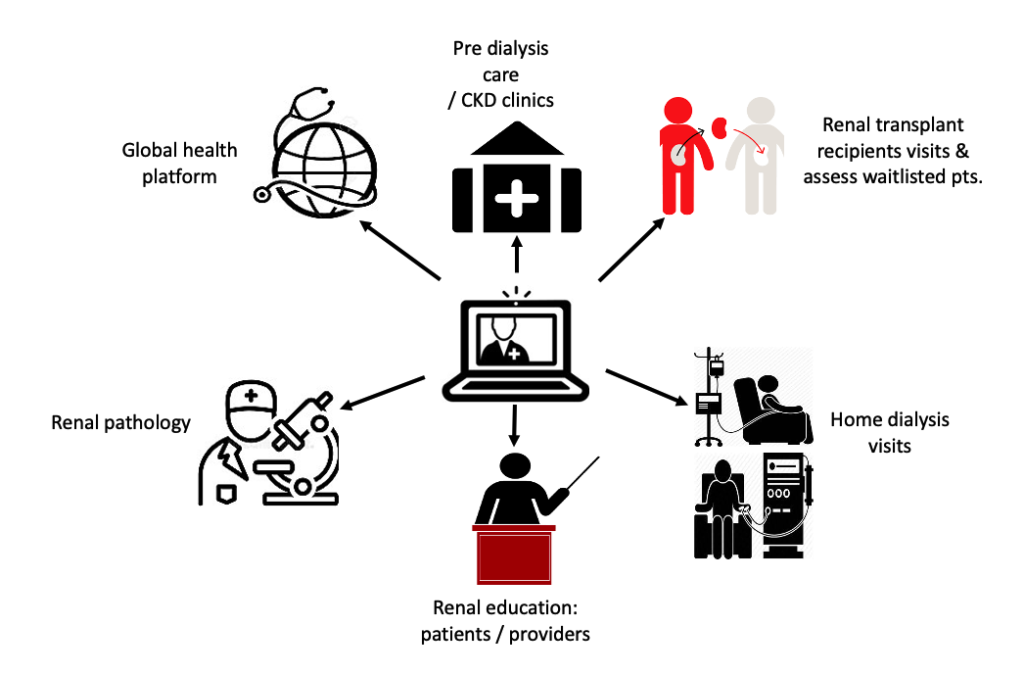
Figure 1. Spectrum of Telemedicine in Nephrology.
Telemedicine, Kidney Education, Pre-Dialysis Chronic Kidney Disease (CKD) Care
Technology has been used to enhance health care delivery for years. The field of nephrology has shown a steady rise in the utilization of technology for patient and care provider education. The domains of Telemedicine and renal education are shown below (Fig.2).

Figure 2. Domains of Telemedicine and Kidney Education
1. Tele-Nephrology Clinic & Pre-Dialysis Care: Narva et al. described successful 9-year implementation of tele-nephrology clinics, providing almost 2,000 patient visits in Pueblo Zuni and Navajo communities in rural New Mexico.
2. Informational websites:
a. Empowering Patients on Choice for Renal Replacement Therapy (EPOCH-RRT) : This decision aid created an adjunct to regular kidney replacement therapy (KRT) education to empower patients with advanced CKD to make appropriate modality decision
b. VA eKidney Clinic: Recent data have demonstrated a tripling of the VA eKidney clinic traffic since its inception in 2013.
3. Mobile applications: “iChoose Kidney” facilitates patient-provider discussions about risks and benefits of transplantation and dialysis. A randomized control trial that looked at the application’s utility found that the iChoose Kidney decision aid improved patient knowledge at evaluation, but did not impact transplant access.
4. Social Media: Both the American Society of Nephrology and the National Kidney Foundation uses Facebook and Twitter as a method of outreach.
5. Multimodality programs: Cricket TM Health Inc. is a technology-aided program which combines educational material, peer support and professional oversight.
6. Virtual support groups: Video conferencing and virtual group education classes (facilitated by health educators or peer leaders) deliver chronic disease education and promote collaborative problem solving, self-reflection and conceptualization. These types of sessions have been tried in chronic diseases like diabetes, but not in the CKD arena yet.
7. Interactive Voice Response (IVR): IVR has immense potential for delivery of CKD education using telephone technology. Its utility is being tested in CKD care.
Telemedicine and Home Dialysis Care Delivery
Home dialysis is underused in the United States and access to these therapies may be impeded by both geographic and socioeconomic factors. To decrease the burden of time required, as of January 2016, CMS approved outpatient monthly capitated payment codes for outpatient peritoneal dialysis care. The various domains of the care are shown in the infographic. The largest barrier to providing telehealth is establishing an appropriate originating site followed by regulatory and reimbursement issues. The University of Alabama established a successful PD telemedicine program in collaboration with the Department of Public Health. Originating sites were set up within the county health departments. Until Jan 2019, Medicare beneficiaries requiring maintenance dialysis were eligible for telehealth only of the originating site was located in a rural area and the patient was placed in an authorized facility (originating site). Beginning 2019, based on the legislation of the 2018 Bipartisan Budget Act, Medicare will pay for a monthly comprehensive telehealth encounter that originates from patients’ home or dialysis unit without geographic restrictions.
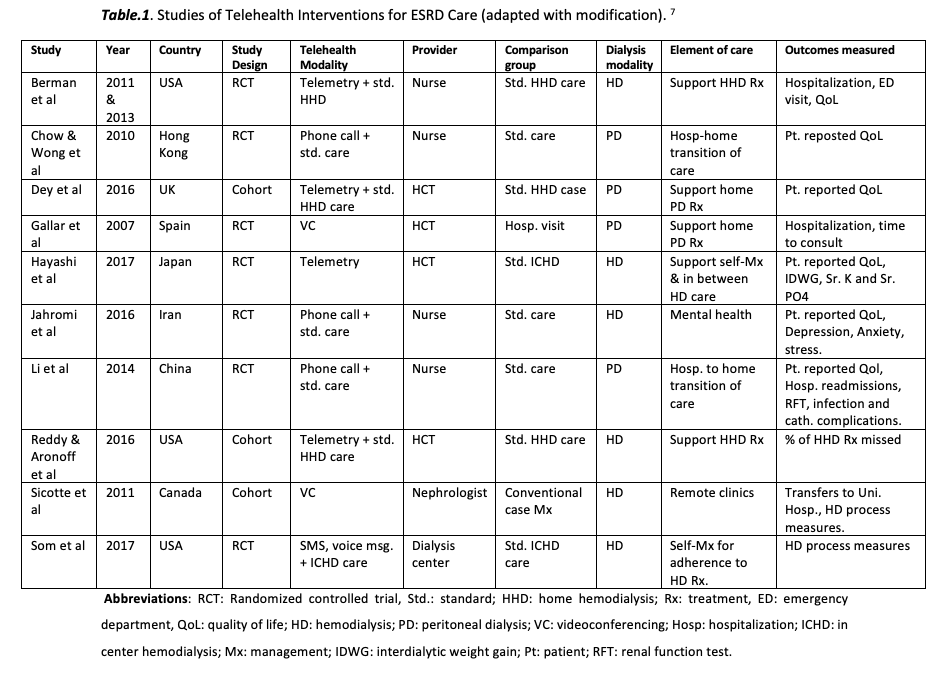
Telemedicine and Quality of Care for End Stage Kidney Disease (ESKD) Patients
A systematic review of literature was conducted to assess the impact of telehealth interventions on processes and quality of care for patients with ESRD. Ten studies were analyzed. Six studies evaluated clinical outcomes, 6 measured patient report QoL. And 5 evaluated impact of telehealth on process of care measures. To summarize, the findings highlighted the potential for telehealth to deliver ESRD care that is comparable to or better than usual care.
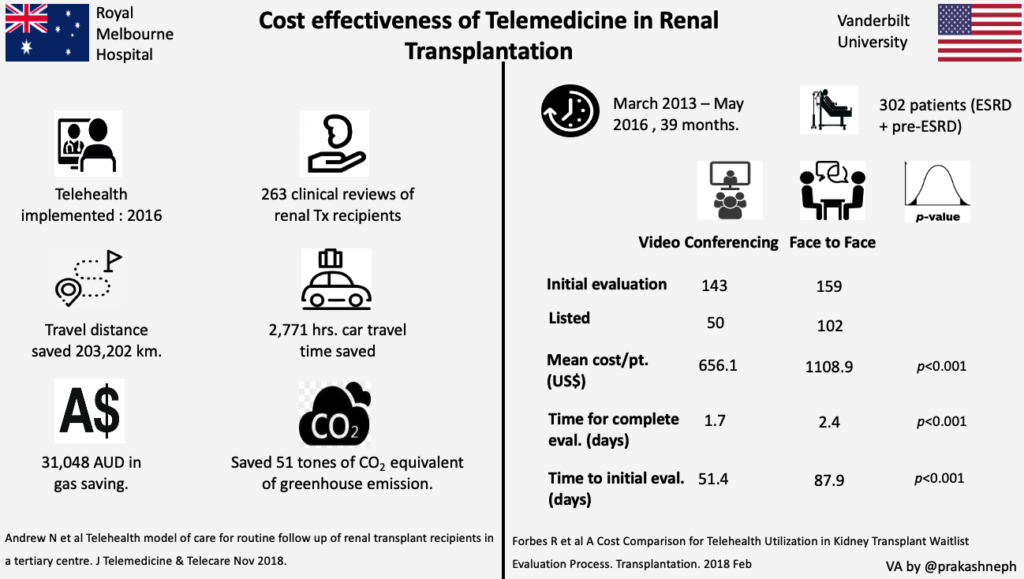
Telemedicine and Kidney Transplant Care Delivery
Barriers to access to renal transplant include referral patterns, timeliness, distance of transplant centers and insurance type. Few institutes are using telehealth to minimize the cost of travel, time to referral and timely follow up of waitlisted patients and renal transplant recipients. The University of Alabama at Birmingham and VAMC Iowa have successfully set up their telehealth program for renal transplant recipients follow up. Preliminary cost analysis data from Royal Melbourne and Vanderbilt / VAMC Nashville has shown promising results (Fig.3).
Telemedicine and Global Kidney Care
Developing countries face many challenges in the delivery of care due to a high incidence of communicable diseases (e.g. Human immunodeficiency virus (HIV), malaria, diarrheal diseases), chronic non-communicable diseases, as well as infrastructural difficulties. Using e-mail and digital image consultations enable prompt consultations. One such platform is “iPath”. It allows clinicians to seek consultations from pathologists globally. This project has been successful in developing countries like Solomon Islands, Egypt, Nigeria, Cambodia and India. Telemedicine makes possible videoconferencing, instant messaging, emails and tele-consults, thereby having the potential to have a large on the global nephrology workforce.
Post by: Prakash Gudsoorkar, University of Cincinnati