Welcome to the 10th case of the Skeleton Key Group, a team of twenty -odd nephrology fellows who work together to build a monthly education package for Renal Fellow Network. The cases are actual cases (without patient identifying information) that intrigued the treating fellow.
Written by: Isabelle Dominique Tomacruz
Visual Abstract by: Denise Arellano
A. The Stem
A 55-year-old post-menopausal female with no known medical or surgical history presents with a three month history of on-and-off, severe, colicky left flank pain radiating to her groin. Three weeks ago, she developed urinary frequency and dysuria. She was prescribed an unknown oral antibiotic which she took for three days, and now her urinary frequency and dysuria are resolved but she continues to have persistent colicky flank pain.
She does not note any polyuria, urinary incontinence or retention, gastrointestinal disturbance or mood changes. She does not take any over-the-counter medications, lithium, vitamins, or herbal supplements. Her family history is unremarkable for kidney stones, cancer or any hereditary or autoimmune disorders.
At clinic, she is asymptomatic and otherwise feels well.
Vital Signs:
Blood Pressure: 110/70 mmHg HR: 78 bpm RR 18/minute Temp: 98.7 °F (37.1 °C) (Oral)
Weight: 55kg Height 157cm BMI 22 kg/m2
Physical examination is only remarkable for left costovertebral angle tenderness.
She shows you baseline labs and a noncontrast CT of the abdomen which was ordered by her primary care physician.
B. The Labs
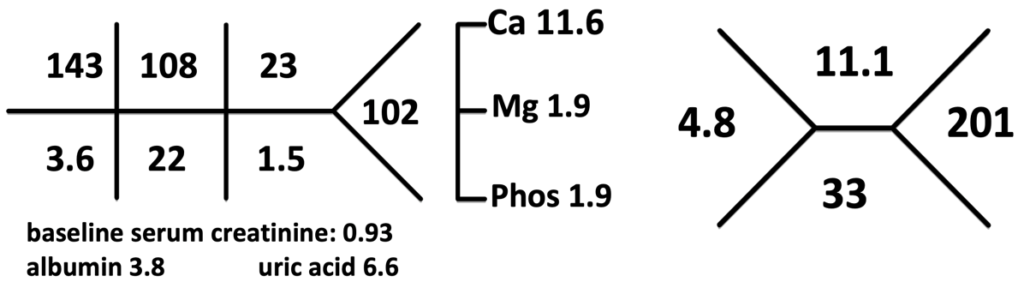
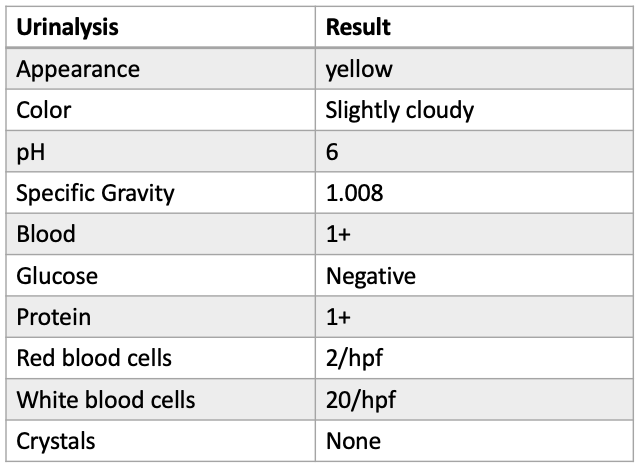
Computed tomography (CT) scan impression:
1. Bilateral nephrocalcinosis (sample photo seen below, Fig 1)
2. Distal ⅓ ureterolithiasis measuring 1.4cm, left
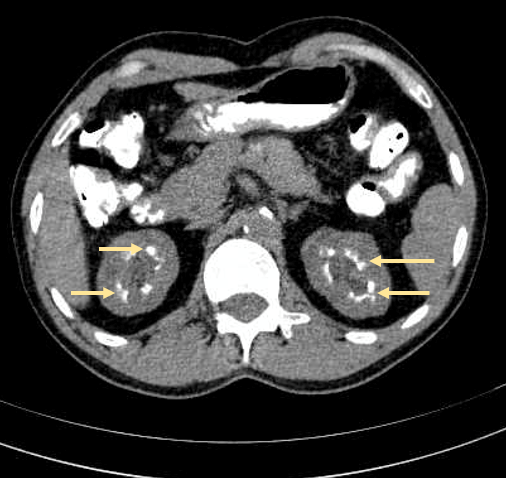
Figure 1. Sample image of bilateral nephrocalcinosis: hyperdense foci in the medulla due to deposition of calcium salts (yellow arrows). Source
C. The Differential Diagnosis: Hypercalcemia
From the initial laboratory results, you immediately notice hypercalcemia.
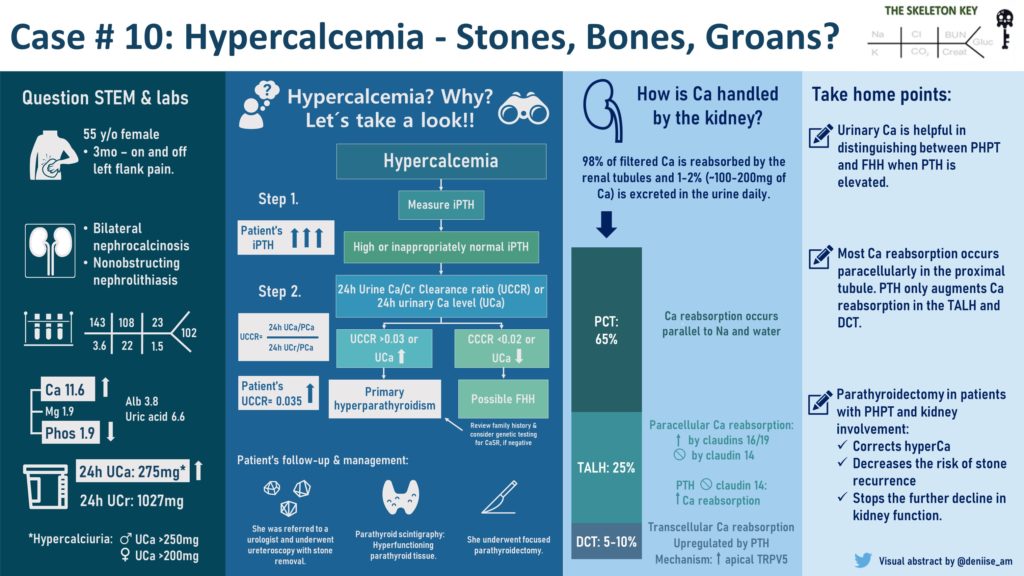
When evaluating hypercalcemia, the first step is to determine if it is parathyroid hormone mediated or non-parathyroid hormone mediated. Here is a diagnostic algorithm (Fig 2) we follow:
D. More Data
Step 1: iPTH (intact Parathyroid Hormone)
In this case, we see that her iPTH is frankly elevated.
Step 2: Urinary Calcium Excretion
Following the algorithm, the differential diagnoses of hypercalcemia and elevated PTH include familial hypocalciuric hypercalcemia (FHH) and primary hyperparathyroidism (PHPT).
Twenty-four hour urine electrolytes will be helpful to differentiate the two. It is also helpful in the evaluation of patients with nephrolithiasis. Of note, the 2014 American Urological Association (AUA) Guidelines on the Medical Management of Kidney Stones recommend initial screening evaluation for new diagnosis of nephrolithiasis and other high risk or recurrent stone-formers.
Let’s take a look at her urine electrolytes:
aUnfortunately 24h urine sodium, potassium, phosphorus, and oxalate was not available for this patient. b24-hour urine creatinine values are also used to assess the completeness of collection. cUCCR is derived from 24-hour urine collection results.
Patients with FHH usually have a positive family history and are asymptomatic with incidental finding of hypercalcemia. This benign condition is caused by an inactivating mutation in the calcium-sensing receptor that leads to increased kidney tubular reabsorption of calcium and consequent low urinary calcium excretion. PTH can be normal or usually only mildly elevated.
Patients with PHPT have hypercalcemia through dysregulated PTH secretion by a parathyroid adenoma or, rarely, a parathyroid carcinoma. Urinary calcium excretion is elevated and PTH is usually elevated or inappropriately normal.
Although there are various definitions for “normal” values in 24-hour urine collections, the most common definition of hypercalciuria is urine calcium >250mg /day in women and >300mg/day in men.
UCCR may be another convenient way to distinguish between FHH and PHPT. Consensus statements have reported that a UCCR> 0.02 have a >90% likelihood of diagnosing PHPT. However some limitations include an elevated UCCR among 20% of patients with FHH, and a low UCCR observed in PHPT patients with vitamin D deficiency or kidney disease. Genetic mutational analysis is helpful among patients with UCCR 0.01-0.02.
E. Final Diagnosis
Our patient was diagnosed with primary hyperparathyroidism (PHPT).
PTH is one of two hormones that regulate calcium balance- the other is calcitriol (1,25-dihydroxyvitamin D). PTH increases calcium reabsorption by:
- stimulating calcium mobilization from the bone (bone resorption)
- increasing calcitriol production leading to enhanced absorption of calcium in the gut
- augmenting passive and active kidney tubular calcium reabsorption in the thick ascending loop of Henle (TALH) and distal convoluted tubule (DCT), respectively
Let’s quickly review kidney calcium handling and PTH:
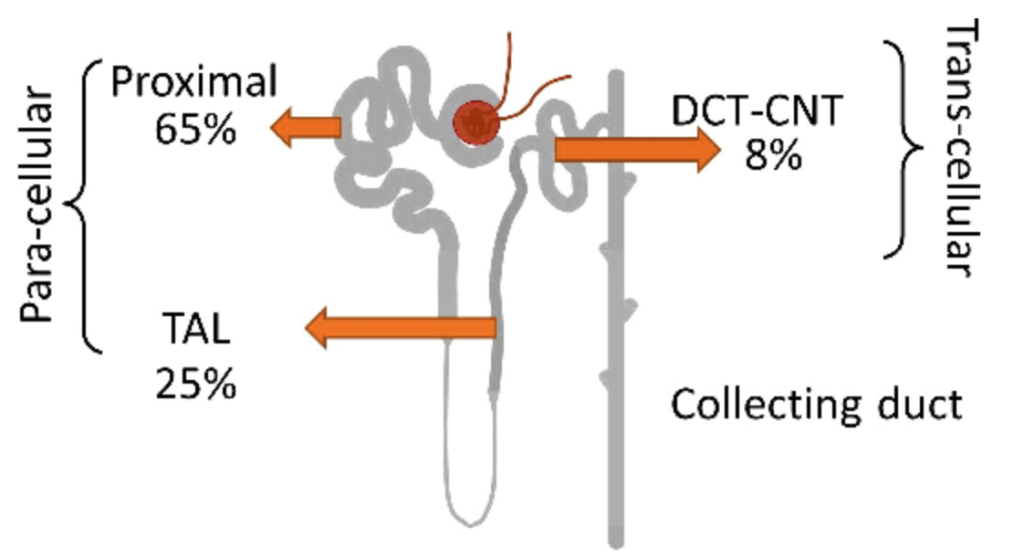
About 98% of filtered calcium is reabsorbed by the kidney tubules and 1-2% (~100-200mg of calcium) is excreted in the urine per day. The majority of reabsorption occurs in the proximal tubule parallel to sodium and water reabsorption (Fig 3).
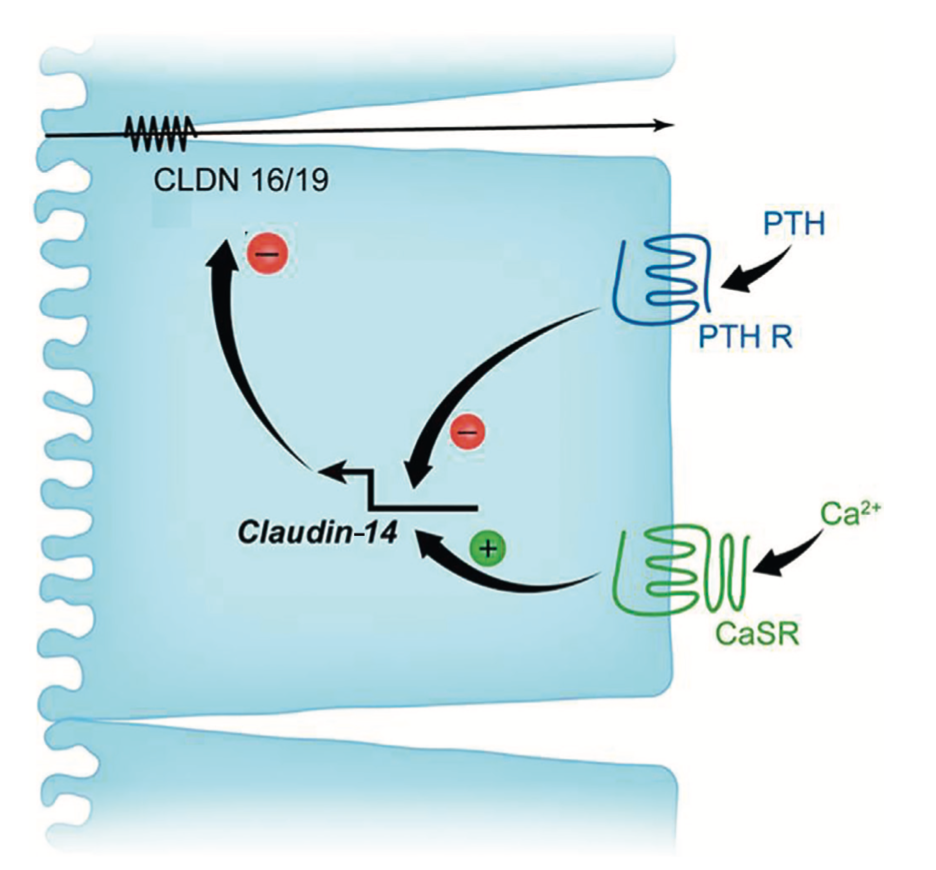
In the thick ascending limb of the loop of Henle, tight junctions express claudin 16/19, which facilitates paracellular calcium reabsorption, and claudin 14, which suppresses it. PTH inhibits the expression of claudin 14 (Fig 4).
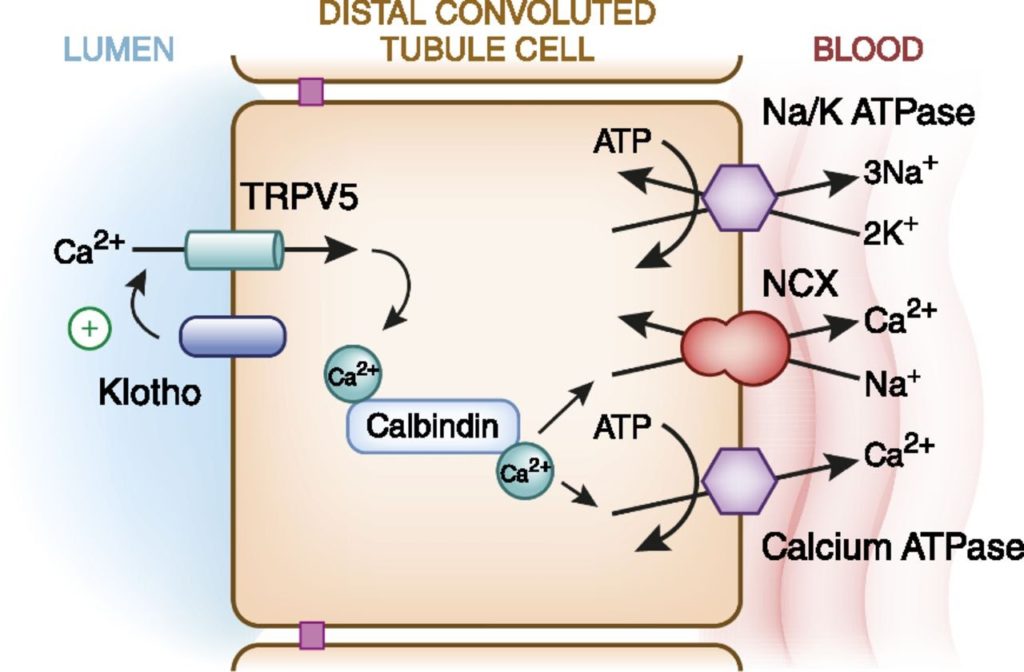
In the distal convoluted tubule, only 5-10% of filtered calcium is reabsorbed exclusively through an active transcellular pathway. Here, PTH binds to a basolateral membrane receptor, stimulating activation of protein kinase A & C pathways, which then lead to increased number and activity of transient receptor potential channels subfamily V (TRPV5) on the apical surface facilitating calcium influx across the apical membrane (Fig 5).
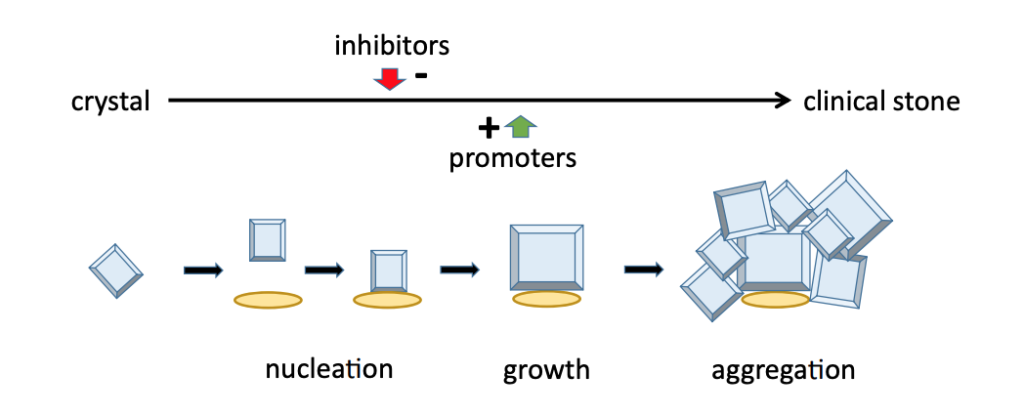
PTH decreases in response to high calcium to result in hypocalciuria. But in PTH-mediated hypercalcemia, the filtered load of calcium outweighs the reabsorptive effect of PTH and results in higher-than-normal levels of calcium excretion. This hypercalciuria is the main risk factor for kidney stone formation (Fig 6). Other risk factors such as hypocitraturia were also seen in our patient.
Going back to our patient, what do we do now?
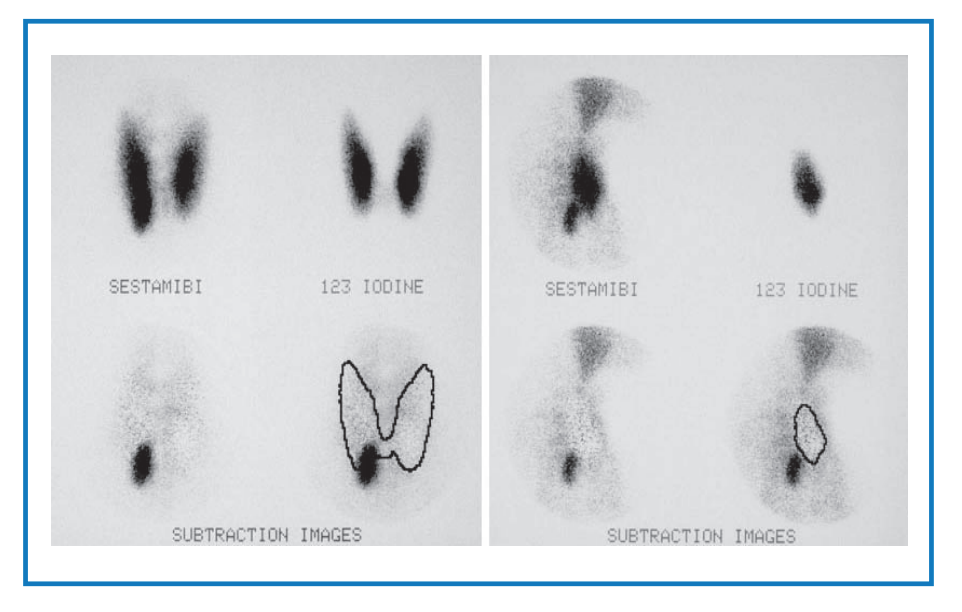
A parathyroid scintigraphy was performed. Results revealed hyperfunctioning parathyroid tissue in the inferior portion of the right thyroid fossa (Fig 7).
PHPT is the most common outpatient cause of hypercalcemia, with an estimated incidence of 50 per 100,000 person-years. Symptomatic kidney stones due to PHPT are now an uncommon finding in developed countries due to an increase in routine biochemical and imaging screening. PHPT and nephrolithiasis must be actively managed to prevent further kidney complications.
F. Management
First, with regard to her nephrolithiasis, she was referred to a urologist and underwent ureteroscopy with stone removal. Her stone composition was 85% calcium oxalate and 15% carbapatite (CaP)
Prevention of recurrent nephrolithiasis relies mainly on correcting the underlying cause. Repeat 24 hour urine electrolytes postoperatively can be helpful in determining if further medical and dietary interventions are needed for the prevention of stones. Medical interventions include adequate fluid intake for a urine volume of 2.5L per day, calcium intake of 1000-1200 mg daily, low sodium diet, the use of potassium citrate for persistent hypocitraturia, or thiazide diuretics in idiopathic hypercalciuria.
High salt intake induces a high sodium load and relative hypervolemia. This results in reduced sodium and water reabsorption, and therefore reduced calcium reabsorption in the proximal tubule. The effect is increased urine calcium and calcium supersaturation. By lowering salt intake we are able to lower urine calcium and therefore lower the risk for kidney stone formation.
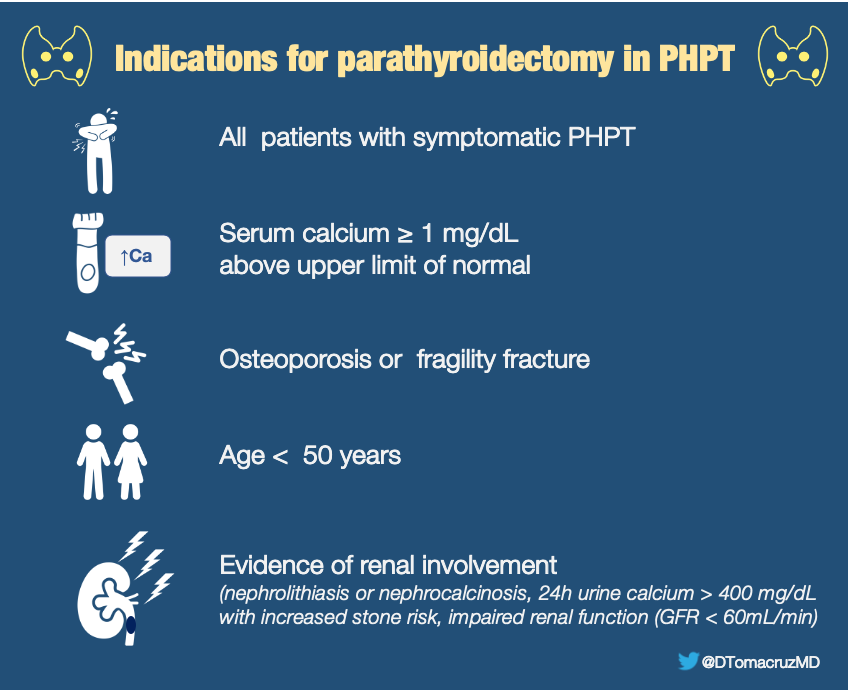
Second & more importantly in the management of our patient, she underwent focused parathyroidectomy. Parathyroidectomy in PHPT is indicated for the following:
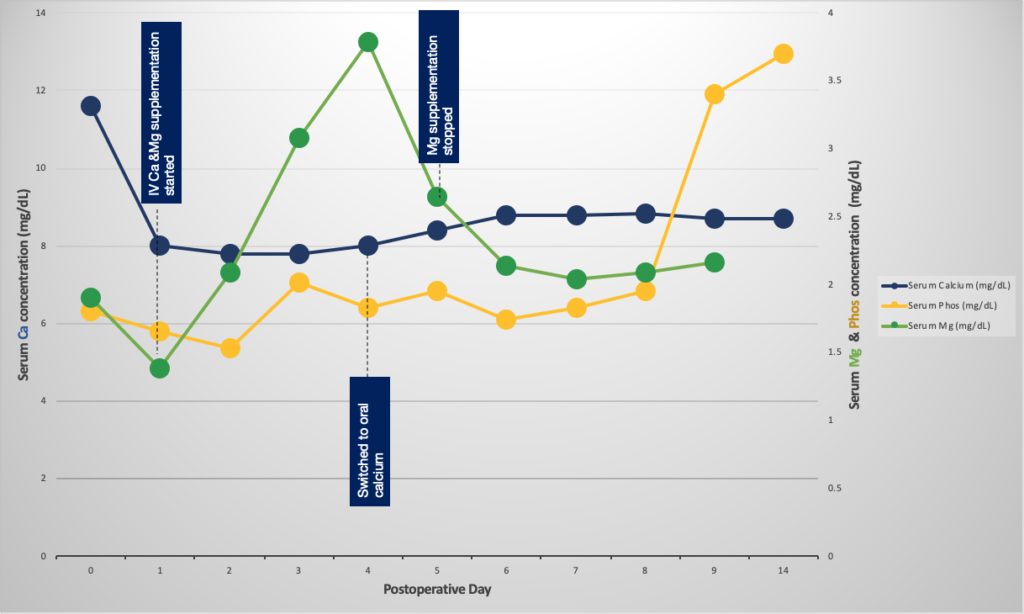
Postoperatively, our patient developed transient hypocalcemia, hypophosphatemia, and hypomagnesemia consistent with hungry bone syndrome, usually seen in those with severe preoperative hypercalcemia and chronic vitamin D insufficiency. Ensuring vitamin D repletion prior to surgery reduces the risk of this complication. Our patient was treated with a short course of calcium and magnesium supplementation, then was shifted to oral calcium supplementation for 2 weeks with careful monitoring of electrolytes upon discharge (See Fig 9). In general, correction of hypophosphatemia is avoided unless severely symptomatic because it may bind with calcium and cause further decrease calcium levels.
Post-parathyroidectomy, acute kidney injury was reversed and serum creatinine remained stable at 1.1mg/dL with correction of hypercalcemia. Her iPTH returned to normal after the procedure and biopsy was consistent with a parathyroid adenoma.
G. Learning Points
- Urinary calcium is helpful in distinguishing between PHPT and FHH when PTH is
- elevated.
- The majority of calcium reabsorption occurs paracellularly in the proximal tubule. PTH only augments calcium reabsorption in the TALH and DCT.
- Successful parathyroidectomy among patients with kidney involvement of PHPT corrects hypercalcemia, decreases the risk of stone recurrence and stops the further decline in kidney function.



Just perfect! So concise and crisp!
Crisp stuff!!! Thank you for putting this up!
Very practical and pathophysiologically detailed approach to this common problem. Congratulations for a job very well done.
Amazing…a perfect quick review.
Excelente presentacion de caso clinico.