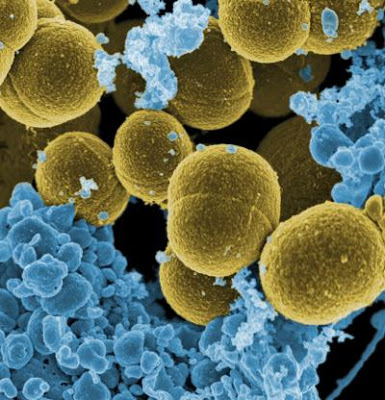
 The two most common organisms causing PD-related peritonitis are (1) Staph aureus and (2) Pseudomonas. Certainly there are other causes–for instance fungal peritonitis (one of the indications for immediate catheter removal) and coagulase-negative Staph species (which usually responds rapidly to antibiotic therapy).
The two most common organisms causing PD-related peritonitis are (1) Staph aureus and (2) Pseudomonas. Certainly there are other causes–for instance fungal peritonitis (one of the indications for immediate catheter removal) and coagulase-negative Staph species (which usually responds rapidly to antibiotic therapy).
As such with suspected peritonitis, before culture results come back, both gram-positive and gram-negative coverage is essential. At our institution (and those with a high rate of MRSA–an ever-increasing problem) the typical cocktail is to give vancomycin plus something for gram-negative coverage–either gentamicin (it’s okay and doesn’t lead to a significant loss of residual renal function if given as a short course) or ceftazidime typically.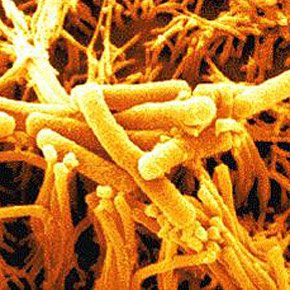 In terms of prophylaxis, an interesting randomized controlled trial (Bernardini et al, JASN 2005) comparing topical gentamicin cream versus mupirocin ointment at the peritoneal catheter exit site was performed. Patients in the gentamicin cream group had a comparable number of gram-positive infections compared to the mupirocin group and a lower rate of gram-negative infections. As a result, gentamicin cream, applied daily, is now recommended as the prophylaxis of choice for peritoneal dialysis patients.
In terms of prophylaxis, an interesting randomized controlled trial (Bernardini et al, JASN 2005) comparing topical gentamicin cream versus mupirocin ointment at the peritoneal catheter exit site was performed. Patients in the gentamicin cream group had a comparable number of gram-positive infections compared to the mupirocin group and a lower rate of gram-negative infections. As a result, gentamicin cream, applied daily, is now recommended as the prophylaxis of choice for peritoneal dialysis patients.
