 Just like there’s no “I” in team…there’s no “N” in ATN.
Just like there’s no “I” in team…there’s no “N” in ATN.
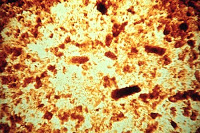
I heard this expression at our Renal Grand Rounds today featuring pathologist Isaac Stillman at nearby Beth Israel Hospital. It’s not completely accurate, as in many cases of ATN, one can often see patchy loss of tubular epithelial cells with resultant gaps and exposure of denuded basement membrane–though recent evidence points to the fact that this is can be the result of either necrosis or apoptosis, a more controlled version of cell death.
But it is true that, despite its name, frank necrosis of renal tubular cells on biopsy is actually fairly rare. ATN remains predominantly a clinical diagnosis, and there are several instances in the literature of patients with a clear diagnosis of ATN who, on renal biopsy, demonstrate a seemingly normal renal histology. Most likely, there is tubular injury, but we just don’t have the sensitivity to detect it. This is supported by recent animal studies identifying various renal biomarkers which are elevated in the urine of virtually all mice subjected to AKI despite apparently normal tubular histology.
When there is necrosis in ATN, it is often most prominent in the outer medulla, where the S3 segment of the proximal tubule joins the medullary thick ascending limb of the loop of Henle, as this is a region already subjected to relative hypoxia. Heavy metal-induced ATN is a special subset of ATN known to demonstrate especially high levels of necrosis than the more common forms of ATN we typically see.


Within the last 2 months. Mercury poisoning. Source of the poisoning is under investigation. The renal failure completely recovered. A very cool case….
Although a fixture in the DDx… When was the last time anyone saw a case of heavy metal induced ATN?!
Cheers