A reduced BUN/Creatinine ratio, an elevated total C02, a low uric acid level, a low Hb (specially if associated with a high ferritin level and a low reticulocyte count), a low cholesterol, a low phosphorus and a low albumin level are the ones which I have found to be most useful. In many outcome studies, several of these abnormalities have been found to be associated with increased mortality.
A low BUN/Creatinine ratio (i.e. characterized by a ratio ≤ 10-15/1) usually implies a low urea generation rate as a result of protein-calorie malnutrition, suboptimal dialysis and/or liver disease.
An elevated or inappropriately normal predialysis bicarbonate level as well as a low uric acid usually denotes the presence of decreased net acid generation as a result of malnutrition.
Low phosphorus, low cholesterol and/or low albumin levels are also seen as the result of malnutrition.
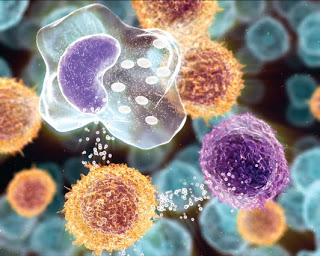
Resistance to the action of erythropoietic stimulating agents is usually suspected in the setting of an unresponsive anemia in conjunction with a hypo-proliferative bone marrow response (i.e. low reticulocyte index). This phenomenon can be the consequence of underdialysis, iron deficiency (as a result of decreased intake-administration, impaired utilization and/or increased losses) and endocrine dysfunction (e.g. hypothyroidism, uncontrolled secondary hyperparathyroidism).
In addition to the etiologies mentioned above, we should also consider (“think outside the box”) that any of them may also be caused by a common denominator – an inflammatory process. In addition to searching for an occult infection (particularly in patients with dialysis catheters), an ischemic skin ulceration, neoplasia, a clotting disorder, etc., we should also think of the retained clotted arteriovenous graft and/or the failed renal allograft as sources of malady! Clarification of their pathogenic role may not be easy as no clinical evidence of a problem (e.g. fever, renal allograft tenderness, hematuria, clotted AV graft warmth-erythema) may be noticeable (specially when patients returning to dialysis with a failed renal transplant are kept on “low dose prednisone”). Markers of inflammation such as an elevated ESR or CRP are useful but not specific. Nuclear studies using radiolabeled WBC’s and/or renal allograft biopsies are not only expensive-invasive but have not always being helpful. Therefore, we must always maintain a high index of suspicion and, if nothing else is found, we should remember that our friendly surgical colleague is just a phone call away!
Posted by Mario Rubin MD


Just an excellent blog you have here. Its very information and I enjoy reading it. I try to visit your blog about twice a week just to see what you have posted 🙂 Keep it up. I was wondering if you can exchange links with me, my blog is http://dialysis-patient-care.blogspot.com, it will really help our Google PageRank and at the same time, it will increase our visitors. I would love to share you stuff to my readers. I went ahead and added your blog to my blogroll, hope you can also do the same.
Sincerly,
Emma
Hemodialysis Patient