 ANATOMY
ANATOMY
The tubulointerstial tissue is composed of cortex and medulla. The cortex has type 1 cells resembling fibroblasts and produces Epo. Type 2 cells in the cortex resemble dendritic cells capable of Ag presentation. Furthermore the cortex contains types 1 and 3 collagen. The medulla has type 1 cells which produce prostaglandins (e.g. COX-2), type 2 cells resembling lymphocytes and type 3 cells located near the vasa recti with unclear function. Histopathologically AIN represents inflamed and edematous interstitium. The phases following such injury include tubular cell proliferation and dilatation, cast formation, atrophy and/or apoptosis and fibrosis.
CAUSES
Tubulointerstitial disease can occur within days to weeks (acute) or within months to years (chronic). There are a lot of (secondary) causes of TIN (tubulointerstitial nephritis) which include:
– Infections: pyelonephritis, vesicoureteral reflux, viral infections (CMV, HCV, HIV, etc.)
– Drugs: NSAIDs, many antibiotics, diuretics, lithium, cidofovir, calcineurin inhibitor, cisplatin, ifosfamide, etc, etc,…
– Toxins: lead, heavy metals, (Chinese) herbs, etc.
– Hem/Onc: multiple myeloma (MM), lymphoproliferative diease, light chain disease, sickle cell disease (SCD), etc.
-Immune-mediated: Sarcoid, Sjogren, SLE, TINU (TIN with uveitis), TIN with hypocomplementemia, etc.
– Genetic: Dent disease, cystinosis, hyperoxaluria, autosomal-dominant hypoparathyroidism, karyomegalic IN, etc.
– Metabolic: hypokalemia, hypercalcemia, urate nephropathy, etc.
– Miscellaneous: Balkan nephropathy, radiation, IBD, etc.
Reference: Braden et al, AJKD, 2005, 46(3)
RENAL FEATURES OF TUBULOINTERSTITIAL NEPHRITIS (TIN)
Electrolyte/Acid-Base disorders:
– Proximal RTA/Fanconi syndrome (MM, SS, Dent disease, cystinosis)
– Distal RTA, type I & type IV: (PN, VUR, Li, Lead, MM, Light chains, SS, SLE)
– Sodium wasting (any disorder)
Clinical syndromes:
– Kidney stones (hypercalcemia, urate, sarcoid, IBD)
– Nephrogenic DI (Li, Cisplatin, hypokalemia, hypercalcemia, Dent)
– ARF (PN, AN, Li, CNI, Cisplatin, Myeloma, Lymphoma, SLE, XRT)
– Papillary necrosis (PN, analgetic nephropathy)
DRUG-INDUCED INTERSTITIAL INJURY
– Time from exposure to development varies
– Sediment: pyuria, WBC casts, eos, hematuria/proteinuria
– One third of patients present with classic symptoms including fever, rash, arthralgias, eosinophilia
– Histologically inflammation with lymphos, monos, eos, plasma cells
– Mechanism: drugs bind to or mimic tubular Ag and cause immune reaction likely through T cells. This causes tubulitis through proinflammatory and profibrotic cytokines
– Most frequent drugs involved: PCN, cephalosporines, phenytoin, thiazide, lasix, cimetidine, ranitidine, rifampin, allopurinol, INF, NSAIDs, COX2 inhibitors (rofecoxib), clarithromycin, PPIs, etc., etc.
– Treatment: DISCONTINUE drug; supportive measures such as maintaining euvolemia andavoidance of nephrotoxins
– Steroids: may help (shorten the time of recovery), but there is no proven benefit in overall outcome
Reference: Choudhury et al, Nat Clin Pract, 2:2, 2/2006
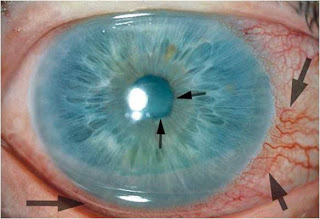
TIN AND TINU (TIN WITH UVEITIS, picture provided on top)
– First described in 1975 by Dobrin and colleagues. Over 200 cases were reported in the literature.
– Patients are mainly adolescents, male to female ratio is 1:3 and median age of onset is 15 (with extremes of 9-74 years of age)
– Risk factors are unclear. Both antibiotics and NSAIDs have been implicated
– TINU Typically presents with ARF and often includes fever, N/V, weight loss, anemia and elevated ESR
– Anterior uveitis (=Iritis) can occur prior, concurrently or after TIN ! In 58-72% of cases it occurs bilaterally.
– Histology often shows activated memory T-cells. An association with HLA-DRB1 has been associated in the literature.
– Adolescents often have spontaneous remission. Steroids often are useful in improving renal function, however Uveitis frequently relapses
References:
Dobrin et al, Am J Med, 59:325, 1975
Takemura et al, AJKD, 34:1016, 1999
Kadanoff et al, J Clin Rheum, 10:25, 2004


