Antiphospholipid syndrome (APS) is an autoimmune hypercoagulable disorder characterized by small-to-large vascular (both arterial and venous) thrombosis with end-organ damages, in presence of circulating antibodies against phospholipid binding proteins.
Kidney transplantation in patients with APS is challenging because post-transplant thrombosis, vascular complications and requirement of anticoagulation during peripoperative period. Let’s start with a brief review of recent advances in transplantation in APS.
For post-transplant TMA due to recurrent APS nephropathy, Canaud et al. recently explored the use of eculizumab. Eculizumab, a humanized mAb that binds C5, prevents cleavage of C5 into C5a and C5b, thereby preventing generation of the membrane attack complex (MAC). At a molecular level, the pathogenesis of endothelial damage in APS is in part via complement activation; C5b-9 MAC deposition on endothelium, leading to cell lysis and/or activation of other proinflammatory pathways, so the use of eculizumab is reasonable. Three patients, maintained with steroids, CNI and MMF, were treated with eculizumab for posttransplant TMA with robust improvement of allograft functions after several doses, and all three patients were successfully withdrawn from maintenance eculizumab treatment after 3-12 months of initial dose. Interestingly, although biopsy showed improved TMA lesions, C5b-9 depositions were persistent for as long as 3 months as “foot prints”. The authors also noticed that eculizumab treatment did not prevent the chronic vascular lesions seen in 12-month protocol biopsies.
Preemptive use of eculizumab in kidney transplant in APS-related ESRD was also attempted in another case series. Three patients, two with CAPS (catastrophic APS), received 1,200 mg of Eculizumab on day 0, 900 mg on POD 1, and weekly thereafter until week 4. After week 5, they received 1200 mg every 2 week. Despite one biopsy proven cellular rejection successfully treated with pulse steroid, graft function and survival was acceptable without recurrence of APS during follow-up of 6 months to 4 years. In the setting of no specific treatment other than systemic anticoagulation, eculizumab seems potentially promising treatment, however, the sufficient treatment length of this drug needs to be optimized, especially due to high cost. Also, there is no description of immunosuppressive regimen either for induction nor maintenance, and it is unclear these patients were on sirolimus or not.
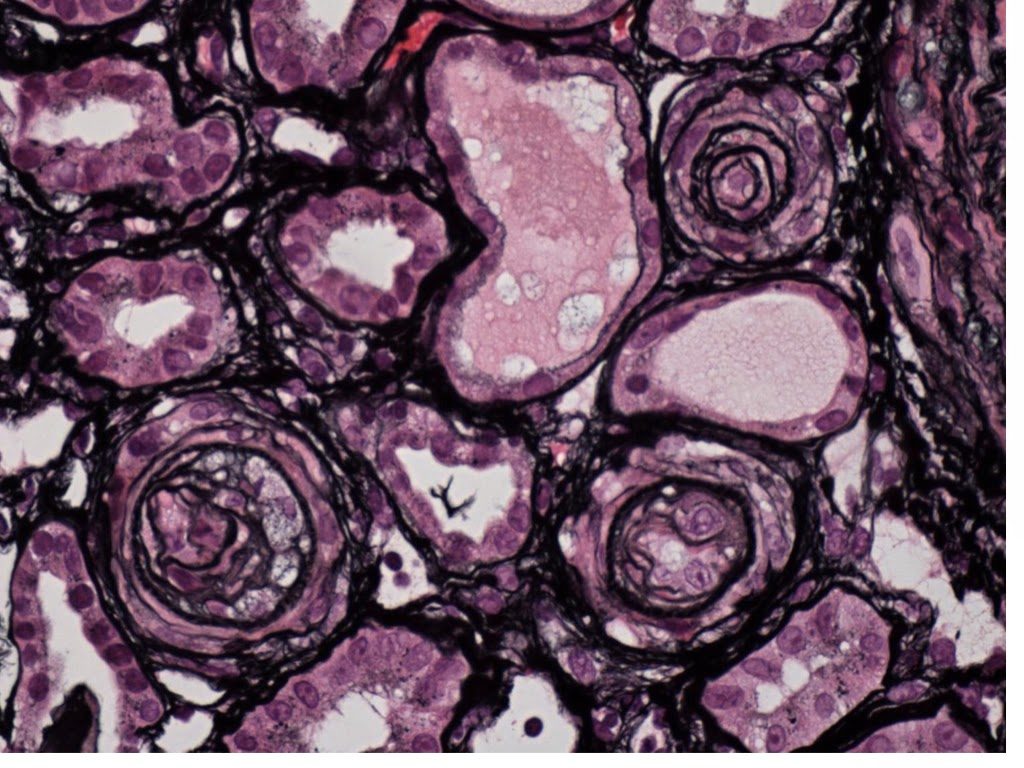
In a recent NEJM article, Canaud et al. indicated the beneficial effect of sirolimus in proliferative vascular changes associated with APS and CAPS, which were not reversed by eculizumab in their previous study. They demonstrated that the chronic vascular changes in APS patients were induced by activation of mTORC via phosphorylation of Akt-S6K pathway, using immunohistochemistry of renal biopsy samples and in vitro signaling studies with HIMEC-1, a human microvascular endothelial cell line, as well as autopsy samples of CAPS. Furthermore, using a cohort of kidney transplant patients with APS (10 treated with steroids+sirolimus+purine inhibitor and 27 with steroids+CNI+purine inhibitor), their nested-case-control study demonstrated that posttransplant allograft functions were better preserved at 144 months post transplant in the sirolimus group compared with CNI group (7 of 10 vs 3 of 27 patients with functioning grafts) and this effect was observed only in patients with APS and not in patients without APS. Other variables including cold ischemia time and immunologic risk profile were comparable between sirolimus and CNI groups.
Although this is a relatively small case-controlled study, the use of mTOR inhibitors for the prevention of APS post-transplant seems very promising.
Naoka Murakami