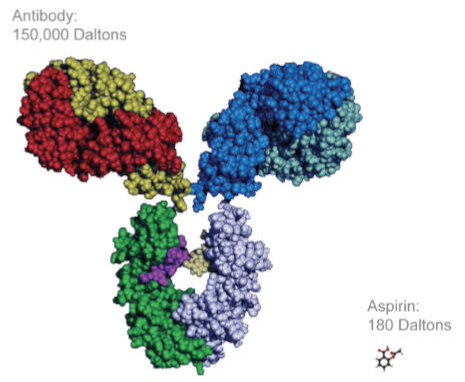
A biopharmaceutical, or biologic, is any medicinal product manufactured in or extracted from a living system, such as a microorganism or plant or animal cells. Several biologic agents are produced using recombinant DNA technology, while others may be manipulated or humanized after their production. Most of these agents are very large and complex molecules compared to traditional small-molecule drugs. Given this fact, the manufacturing process of biologics is more challenging than traditional drugs, as even minor changes in the manufacturing process can impact efficacy or immunogenicity.
Use of biologic agents is now commonplace in many disease states, including oncology, rheumatology, renal transplant and nephrology. One of the major limitations of use of these agents is their associated costs. A small molecule drug costs, on average, $1/day, with generic drugs often costing just cents. In comparison, a biological drug costs, on average, $22/day. It is estimated that global biological sales are projected to reach $221 billion by 2017. One way to limit the healthcare expenditure on biologic agents is to allow for competition within the marketplace. However, given the complex manufacturing processes involved in making biologics, the Food and Drug Administration (FDA) has traditionally not allowed generic competition for these products, even after their patents have expired. This all changed on March 23, 2010 when the Patient Protection and Affordable Care Act was signed into law. This created an abbreviated licensure pathway for biological products that are demonstrated to be “biosimilar” to or “interchangeable” with approved, reference biological agents.
A biosimilar is simply defined as a biopharmaceutical protein designed to have active properties similar to an innovator biologic and approved through an abbreviated regulatory process. Due to the complexity of the manufacturing process, biosimilars should not be considered generic versions of biologics. The FDA requires animal studies to assess toxicities, as well as human pharmacokinetic (PK) and clinical studies prior to approval of a biosimilar product. The objective of the PK study is to demonstrate comparability of relevant parameters in a sufficiently sensitive and homogeneous population. This analysis is often done in concert with the clinical study. For the clinical study, the primary objective is to establish biosimilarity, not clinical benefit, as its efficacy is already known from the registration studies of the innovator product. Biosimilarity is often established through a randomized, parallel group, comparative clinical trial.
The FDA has published “The Purple Book” that contains a list of licensed biologic products to help clinicians see whether a particular product has been determined by the FDA to be biosimilar to, or interchangeable with, a reference biologic product. Despite the approval pathway for biosimilars being signed into law over five years ago, it was not until March 2015 that the FDA approved the first biosimilar product, Zarxio® (filgrastim-sndz).
Biosimilars are a relatively new in the US; however, the European Medicines Agency (EMA) has had a regulatory process for approval of biosimilars for nearly 10 years. Their approvals for biosimilars cover five classes: recombinant erythropoietins (i.e., epoetin alfa, epoetin zeta); recombinant granulocyte-colony stimulating factors (i.e., filgrastim); recombinant human growth hormone (i.e., somatropin); recombinant follicle stimulating hormone (i.e., follitropin alfa) and monoclonal antibodies (i.e., infliximab). To date, the EMA has approved 19 biosimilars.
Biosimilars are a relatively new in the US; however, the European Medicines Agency (EMA) has had a regulatory process for approval of biosimilars for nearly 10 years. Their approvals for biosimilars cover five classes: recombinant erythropoietins (i.e., epoetin alfa, epoetin zeta); recombinant granulocyte-colony stimulating factors (i.e., filgrastim); recombinant human growth hormone (i.e., somatropin); recombinant follicle stimulating hormone (i.e., follitropin alfa) and monoclonal antibodies (i.e., infliximab). To date, the EMA has approved 19 biosimilars.
Biosimilars in Nephrology
After 6 years of successful use in Europe, data has demonstrated that biosimilar erythropoiesis-stimulating agents (ESAs) are safe and effective alternatives to brand-name epoetin alfa for treating anemia in patients with kidney disease. In United States, the patent for Procrit® (epotein alfa) expired in August 2013; however, the patent for Epogen® (epoetin alfa) remains active until May 2015. On the other hand, the patency for Aranesp® (darbapoetin alfa) will expire in 2024. Since the U.S. key patents on epoetin alfa have begun to expire, Hospira has submitted Biologics License Application to U.S FDA to get Retacrit® (epoetin zeta) approved as a proposed biosimilar for epoetin alfa.
Biosimilars in Transplantation
Monoclonal antibodies are very complex biologics that have shown to be effective for different indications. In renal transplantation, a series of monoclonal antibodies have been used as induction therapy or to treat steroid-resistant acute rejections, such as Simulect® (basiliximab) or Campath® (alemtuzumab). It appears that alemtuzumab will lose patent protection at the end of 2015, while basiliximab patent protection will expire in 2018. These could be among the first transplant-related immunosuppressive biosimilars approved in the US within the next five years.
–
Razan M. Alsheikh, PharmD, BCPS, PGY-2 Organ
Transplant Pharmacology Resident, Brigham and Women’s Hospital, Boston, MA
Razan M. Alsheikh, PharmD, BCPS, PGY-2 Organ
Transplant Pharmacology Resident, Brigham and Women’s Hospital, Boston, MA
–
Steven Gabardi, PharmD, FCCP,
BCPS, Department of Transplant Surgery and Renal Division, Brigham and Women’s
Hospital, Boston, MA
Steven Gabardi, PharmD, FCCP,
BCPS, Department of Transplant Surgery and Renal Division, Brigham and Women’s
Hospital, Boston, MA