 I
Irecently finished my 2nd month on the consult service which was a
very exciting time for me because I saw patients with every class of Lupus with
different kinds of presentations. It was especially rewarding because I
biopsied majority of these patients myself and then followed their course
through diagnosis, initiation of immunosuppression and witnessed improvement in
subsequent clinic visits. I find Lupus Nephritis most fascinating among all the
GNs.
One
of the most interesting cases I saw since the beginning of fellowship was of a
36 yrs. old woman who presented with joint pain, malar rash, photosensitivity,
worsening generalized edema and nephrotic range proteinuria of 8 grams. She had
2 prior renal biopsies- one with a diagnosis of Minimal Change Disease and the
second one 2 years ago with FSGS tip lesion and Class 2 lupus Nephritis.
of the most interesting cases I saw since the beginning of fellowship was of a
36 yrs. old woman who presented with joint pain, malar rash, photosensitivity,
worsening generalized edema and nephrotic range proteinuria of 8 grams. She had
2 prior renal biopsies- one with a diagnosis of Minimal Change Disease and the
second one 2 years ago with FSGS tip lesion and Class 2 lupus Nephritis.
On
her current presentation, she met the ACR criteria of diagnosis of SLE. We
biopsied her again and essentially found the exact same lesion- FSGS tip lesion
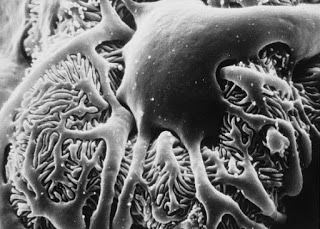
with Class 2 lupus nephritis. There were
only scant mesangial deposits, no endocapillary proliferation or necrosis and
weak but full house staining on IM. EM showed diffuse foot process effacement.
We diagnosed her with Lupus Podocytopathy and she was started on high dose
steroids and immunosuppression with MMF with subsequent rapid resolution of
symptoms and proteinuria to 0.8 grams within 2 weeks. It remains to be seen how
she continues to respond to the treatment and if she remains in remission. She
still is likely to relapse in future and switch to a different class of lupus
nephritis along her course.
her current presentation, she met the ACR criteria of diagnosis of SLE. We
biopsied her again and essentially found the exact same lesion- FSGS tip lesion
with Class 2 lupus nephritis. There were
only scant mesangial deposits, no endocapillary proliferation or necrosis and
weak but full house staining on IM. EM showed diffuse foot process effacement.
We diagnosed her with Lupus Podocytopathy and she was started on high dose
steroids and immunosuppression with MMF with subsequent rapid resolution of
symptoms and proteinuria to 0.8 grams within 2 weeks. It remains to be seen how
she continues to respond to the treatment and if she remains in remission. She
still is likely to relapse in future and switch to a different class of lupus
nephritis along her course.
Podocytopathy
is a glomerular disease which occurs due to extrinsic or intrinsic primary
podocyte injury. Lupus Podocytopathy occurs in association with new or relapse
of SLE signs and symptoms.
is a glomerular disease which occurs due to extrinsic or intrinsic primary
podocyte injury. Lupus Podocytopathy occurs in association with new or relapse
of SLE signs and symptoms.
It
is a rare presentation of Lupus Nephritis – the reported incidence is 1.33% of patients
with Lupus Nephritis. So far there have been 22 reported cases in literature.
Up until the early 2000s, nephrotic syndrome in a patient with class 2 lupus
was deemed as a coincidence. The work of
Dube et al,
Hertig et al and Kraft et al lead to an understanding that the appearance
of nephrotic syndrome in a patient with Class 2 lupus (without any
endocapillary proliferation or GBM deposits) coincided with Lupus flare or
appearance of Lupus symptoms. Among these patients, the nephrotic syndrome
appears best correlated with podocytopathy rather than subepithelial electron
dense deposits, mesangial deposits, or mesangial hypercellularity. The
currently used ISN/RPS classification of Lupus Nephritis does not include Lupus
Podocytopathy.
is a rare presentation of Lupus Nephritis – the reported incidence is 1.33% of patients
with Lupus Nephritis. So far there have been 22 reported cases in literature.
Up until the early 2000s, nephrotic syndrome in a patient with class 2 lupus
was deemed as a coincidence. The work of
Dube et al,
Hertig et al and Kraft et al lead to an understanding that the appearance
of nephrotic syndrome in a patient with Class 2 lupus (without any
endocapillary proliferation or GBM deposits) coincided with Lupus flare or
appearance of Lupus symptoms. Among these patients, the nephrotic syndrome
appears best correlated with podocytopathy rather than subepithelial electron
dense deposits, mesangial deposits, or mesangial hypercellularity. The
currently used ISN/RPS classification of Lupus Nephritis does not include Lupus
Podocytopathy.
A
more recent article in CJASN in April 2016 studied
a cohort of 50 Chinese SLE patients (the largest so far) with diffuse Foot
Process Effacement and class 1 and 2 lupus nephritis. They included minimal change disease (MCD) in 13 cases, mesangial
proliferation in 28 cases, and FSGS in nine cases.They have proposed a list of criteria to
diagnose Lupus Podocytopathy and suggest revision of ISN/RPS classification of
Lupus nephritis to include Lupus podocytopathy as a distinct entity. The
immunologic and molecular mechanism of Lupus podocytopathy has not yet been
fully studied but the T-cell abnormalities in both the disorders could be the
unifying pathogenic mechanism in the occurrence of MCD or FSGS in SLE.
more recent article in CJASN in April 2016 studied
a cohort of 50 Chinese SLE patients (the largest so far) with diffuse Foot
Process Effacement and class 1 and 2 lupus nephritis. They included minimal change disease (MCD) in 13 cases, mesangial
proliferation in 28 cases, and FSGS in nine cases.They have proposed a list of criteria to
diagnose Lupus Podocytopathy and suggest revision of ISN/RPS classification of
Lupus nephritis to include Lupus podocytopathy as a distinct entity. The
immunologic and molecular mechanism of Lupus podocytopathy has not yet been
fully studied but the T-cell abnormalities in both the disorders could be the
unifying pathogenic mechanism in the occurrence of MCD or FSGS in SLE.
There
is very limited data currently on the treatment of this group of patients as
almost all of it comes from observational studies. But so far, we know that
patients with Lupus Podocytopathy are highly steroid responsive. Those who have
an FSGS lesion are prone to more relapses and incomplete remission as compared
to the ones with MCD, and also need immunosuppressive agents with steroids. Both
nephrologists and renal pathologists need to be aware of this entity as a cause
of nephrotic syndrome in patients with SLE
is very limited data currently on the treatment of this group of patients as
almost all of it comes from observational studies. But so far, we know that
patients with Lupus Podocytopathy are highly steroid responsive. Those who have
an FSGS lesion are prone to more relapses and incomplete remission as compared
to the ones with MCD, and also need immunosuppressive agents with steroids. Both
nephrologists and renal pathologists need to be aware of this entity as a cause
of nephrotic syndrome in patients with SLE
Posted by Manasi Bapat, Nephrology Fellow, Mount Sinai Hospital, NY


This commentry nicely depicts the importance of incorporating Lupus podocytopathy as a distinct group of the lupus classification. However, some people also include collapsing glomerulopathy in lupus patients, but i think it is important to keep these separate as the minimal change-like podocytopathy responds really well to steroids and collapsing glomerulopathy probably has a very different background (possibly related to APOL1 variants, as both SLE and collapsing GP are more common in blacks).