Welcome to the 7th case of the Skeleton Key Group, a team of twenty odd nephrology fellows who work together to build a monthly education package for Renal Fellow Network. The cases are actual cases (without patient identifying information) that intrigued the treating fellow.
Written by: Sudha Mannemuddhu
Visual Abstract: Anna Gaddy
It’s acidosis again… this time it has the flavors of three worlds: Nephrology, Gastroenterology, &Urology. Let’s see if you can solve the puzzle… challenge accepted?!
A. The Stem
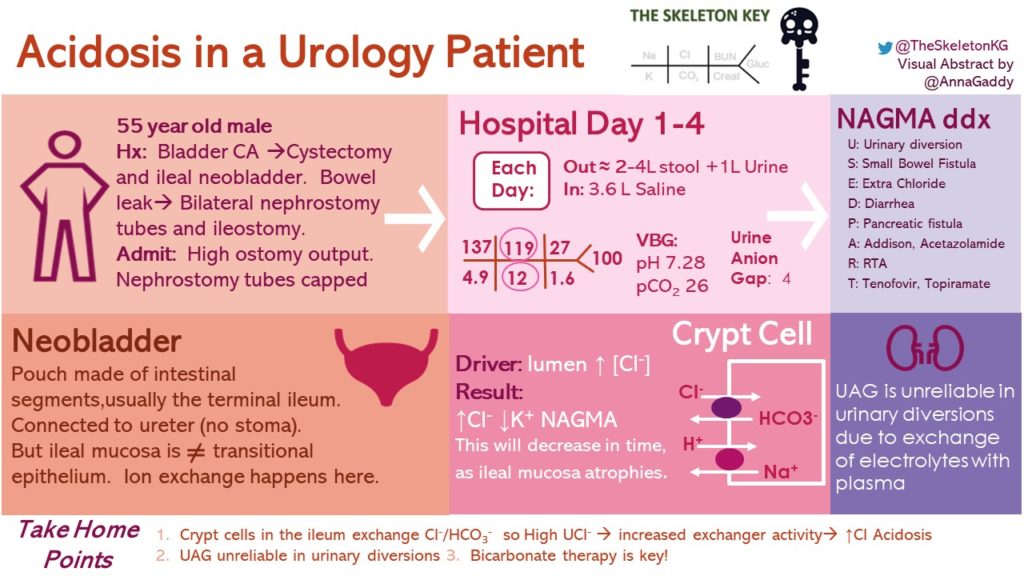
A 55 year old man with a history of urothelial cancer underwent transurethral resection of the tumor, radical cystectomy and neobladder construction. Surgery was complicated by urinary and bowel leak requiring bilateral diverting percutaneous nephrostomies (PCNs) and ileostomy placement. He presented to the clinic three months postoperatively with persistently high ostomy output (over 4 L/day). He states it is more watery the past few days associated with lightheadedness and decreased energy.
He has tried multiple therapies, including loperamide and atropine/diphenoxylate, without much success. He was hospitalized in order to decrease his ostomy output and to assess him for an ileostomy reversal. The team is calling you for worsening acidosis during his hospitalization, and his bilateral PCNs have been capped.
He does not report having fever, chills, abdominal pain, heartburn, increased oral intake, or change in his diet.
Vitals:
Blood Pressure: 117/74 mm of Hg
HR: 73 bpm
RR: 18/min
O2 sat 100% on room air
Temp: 97.7 F
Wt: 80 Kg
Physical Examination:
General: NAD, alert and oriented x3, fatigued
Head and Neck: Extraocular movements intact, moist mucous membranes, no jugular venous distension
Heart: Regular rhythm, normal S1/S2, no rubs, murmurs, or gallops
Lungs: Clear to auscultation bilaterally
Abdomen: Soft, non-tender, non-distended, normoactive bowel sounds Ileostomy: Watery fecal material, no blood
Current medications are listed below:
- Long acting insulin 25 units daily
- Rosuvastatin
- Omeprazole 20 mg daily
- Loperamide 2 mg, every 6 hours
B. The Labs
Venous blood gas (VBG) showed pH 7.28, pCO2 26 mmHg…Normal Anion Gap Metabolic Acidosis (NAGMA)…Anion gap = 6 (8.3, when corrected for albumin of 3.1 mg/dL)
C. Differential Diagnosis: Hypomagnesemia
Differential Diagnosis for Non-Anion Gap Metabolic Acidosis (NAGMA)
HARDUP
H: Hyperchloremia, Hyperparathyroidism
A: Addison’s, Ammonium Chloride
R: RTA
D: Drugs (Acetazolamide, Tenofoivir, Topiramate), Diarrhea
U: Ureterosigmoidoscopy
P: Pancreatic fistula
USED PART
U: Urinary diversion/ Ureteroenterostomy
S: Small Bowel Fistula
E: Extra Chloride
D: Diarrhea
P: Pancreatic fistula
A: Addison, Acetazolamide
R: RTA
T: Tenofovir, Topiramate
Let’s take a look at our case work through the possible contributors…
- Ileostomy losses – Potassium should be usually low, and urine electrolytes may help provide an answer
- Kidney losses – The patient may have a possible renal tubular acidosis (RTA). Perhaps the neobladder is responsible?
- Normal Saline (NS) administration – Contributing factor
D. More Data
He has been in the hospital for 8 days now, and his serum bicarbonate level has been decreasing each day. During his hospitalization, he was started and continued on 0.9% NS at 150 mL/hr to keep up with his ostomy outputs. His ostomy output since admission was recorded around 2-4 L/day.
His blood work shows the following:
Urine Anion Gap (UAG): [Na+] + [K+] − [Cl-] (concentrations are expressed in mEq/L) = 65 + 33 – 94 = + 4
Things to pay attention here:
- Ileostomy output has been decreasing during the hospitalization with anti motility regimen with loperamide, psyllium husk etc, but his acidosis is worsening,
- His diverting PCN’s were capped five days ago, and will be taken out soon.
- He has been voiding through his neobladder since his hospitalization.
E. The Answer: NAGMA, Due to the Neobladder
What is a neobladder?
It is one of the commonly used urinary diversion procedures as depicted in Figures 1a and 1b . Neobladder is constructed using intestinal segments (Ileum, colon and sigmoid and rarely jejunum or gastric tissue), most commonly terminal ileum due to its capacity and distensibility, as well as due to that fact that mucosal atrophy is seen in ileum in the long run.
Contraindications of neobladder construction are:
- Patients who are high risk for cancer recurrence
- Patients that are not motivated or unable to self cath
- Impaired sphincter or incompetent urethra.
- patients with active intestinal disease (because you need more ileal tissue for a neobladder than an Ileal conduit)
Now that we learned almost everything about surgery, let’s get back to our fun world of numbers (Figure 2):
But you told me that a positive UAG is a kidney issue. Does his UAG of 4 mean anything?
With shifts of fluid and electrolytes between ileal mucosa and the bloodstream as described below, urine collected from the neobladder is unreliable. Moreover the UAG level of 4 itself is not reliable. Look for a positive UAG between 20 to 90, and a negative UAG between -20 to – 50. More details in our prior RFN post.
And what about all of that 0.9% NS he received?
The patient received around continuous 0.9% NS, around 3.6L per day, since Nephrology was consulted. Upon consultation, the fluids were changed to a D5W with 150 mEq of sodium bicarbonate. It is likely his acidosis was further worsened by administration of chloride rich fluids.
F. A Few More Words on the Neobladder
Why do neobladders cause electrolyte abnormalities?
The urine is rich in potassium, hydrogen and chloride, which is exchanged with sodium and bicarbonate in the blood causing hyperchloremic, hypokalemic metabolic alkalosis. Let’s look at the cells and acid-base transport systems across the ileum. There are predominantly two types of cells in ileal villi and crypts as shown in figure 3.
What is the role of these acid base systems in the ileum?
In ileum, Na+/H+ exchanger maintains pH thereby allowing NaCl to be a major driving force for fluid absorption in the intestine. Apical Cl–/HCO3– exchanger plays a pivotal role in bicarbonate secretion.
I know what you are thinking, there is a similar cell in the kidney! You are right, It’s the intercalated cell in the distal collecting tubule.
Apical Cl–/HCO3– exchanger in the ileal cell functions just like collecting duct exchanger and secretes HCO3– into the neo bladder lumen. Excess Cl–, K+ and H+ in the urine from the neobladder exchanges with Na+ and HCO3– from the bloodstream, causing hyperchloremic metabolic acidosis. Nevertheless, mucosal atrophy overtime can decrease these electrolyte imbalances.
Because this is gut tissue we’re talking about, it can also reabsorb creatinine, urea, and ammonia, which is part of the reason why neobladders are discouraged in patients with kidney or liver disease.
Does it matter how much ileum is taken? Yes, it does.
Ileum is the 3rd segment of the small intestine and is about 150 cm in length. Duodenum and jejunum are 25-30cm and 100 cm respectively. Ileum is the site of absorption for 8-9 L of fluid, vitamin B12, and bile salts. The ileum and colon are also the main sites for Cl absorption in exchange for bicarbonate, contrary to the jejunum where bicarbonate is preferentially absorbed.
More than 100 cm resection of ileum can cause 3 major long term complications of chronic bile salt wasting and fat malabsorption are renal stones, bone disease (osteoporosis and osteomalacia), and gallstones. In addition, feedback detection of malabsorption via peptide YY and GLP1 are impaired.
How much tissue is taken for ileal conduits and neobladders?
Ileal conduits typically utilize around 20 cm of ileal tissue. A neobladder uses around 40-60 cm of ileal tissue. Care is given to avoid the ileocecal valve (around 20-25 cm away) in order to avoid worsening metabolic acidosis from osmotic diarrhea and decreased fecal transit time. Although there are now modified ileal neobladder procedures which use as little as 25 cm of the ileal segment.
Will our patient have acidosis forever? And if not, then what are the risk factors for persistent acidosis?
It is unlikely, although our patient does have risk factors which indicate he will likely have a persistent metabolic acidosis. Conditions which allow more time for exchange to occur are more likely to result in persistent metabolic acidosis, such as urinary obstruction, stasis, or increased urinary residual volume. Interestingly, a study of patients at a rehabilitation facility post-ileal neobladder found that the risk of metabolic acidosis increased as a patient’s continence improved.The need for sodium bicarbonate therapy increased during the rehabilitation stay from 45.2% of patients to 86.7% of patients. This was seen during the same time period that urine loss (ie incontinence) was reduced.
Over time, the rate of metabolic acidosis with an ileal neobladder decreased. In one study the incidence went from 52% at one month, to 19.5% at one year, and 7.3% at two years. Loss of exchangers due to mucosal atrophy is the proposed reason. Risk factors for persistent metabolic acidosis varied over time, with impaired renal function being important at one month (OR 3.87), while diabetes was important at 1- and 2-years withs odds ratios of 5.68 and 7.62 respectively.
One would assume that patients with neobladder may have higher incidence of metabolic acidosis compared to ileal conduits given the increased length of ileal tissue used, but in a study of patients who received ileal neobladders or ileal conduits, although more patients with an ileal neobladder had metabolic acidosis (31%) compared to ileal conduit (14.8) at one month and at one year (22.9% with ileal neobladder and 10% with ileal conduit) had no statistical difference.
Take Home Messages
What happened to our patient? After capping and subsequently removing the PCNs, his urine output from the neobladder was stable at around one liter per day, and with antimotility and bulking agents his ileostomy output decreased to a liter per day. He was started on 1300 mg of sodium bicarbonate tablets, twice a day and within 2 days his labs returned normal and he was discharged home.
- Urine electrolytes are sometimes helpfu,l but not in case of UAG in the setting of neobladder or ileal conduit systems due to exchange of electrolytes with plasma
- The apical Cl–/HCO3– exchanger plays a major role in the development of metabolic acidosis when ileal tissue i
- s used.
- Though this can be transient…urinary obstruction, stasis, increased urinary residual volume, and/or short gut syndrome can worsen and prolong acidosis
- Bicarbonate replacement is the most commonly used therapy



will look into it. Thanks for pointing out.
This key is broken! Please fix
Interesting case and good introduction to the spectrum of urinary diversions. I am intrigued by the hypokalemia accompanying the met acidosis. What could be the physiology?