Saw a patient today in clinic who was s/p simultaneous pancreas-kidney transplant about 15 years ago.
The kidney is hanging in there (Cr 2.5mg/dl) and the patient does not require insulin, so we have to consider the transplant a success. However in going through her medication list, I noticed that the patient was on massive doses of oral sodium bicarbonate, plus they have instructions to take oral salt tablets during the summer months. What does this tell us about pancreas transplant?
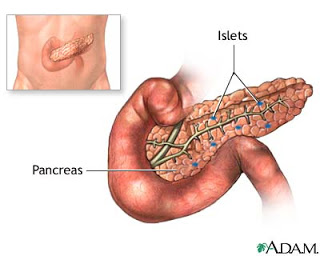
Drainage of the exocrine contents of the transplanted pancreas can be achieved surgically in two different ways: either bladder drainage or enteric drainage.
Bladder drainage is apparently technically easier, and initial reports suggested fewer pancreatic allograft failures using bladder drainage than with enteric drainage. In addition, bladder drainage also allows for monitoring of urinary amylase levels, which can be used as a marker for pancreatic transplant rejection (monitoring rejection of pancreatic allografts is more difficult than rejection of kidney allografts, where one can use creatinine as a relatively sensitive marker for rejection…by the time blood sugars begin to rise as a result of pancreatic rejection, it’s basically game over and the pancreas can’t be rescued by increasing immunosuppression). However, one of the main side effects of bladder drainage of the pancreatic exocrine fluid is that it leads to a situation of unregulated sodium and bicarbonate loss. These patients are quite sensitive to hypovolemia (as they cannot retain sodium like a normal kidney can) and can develop chronic metabolic acidosis. Thus, our patient had been given a pancreatic transplant with bladder drainage, which accounts for her dependence on salt tablets and oral bicarbonate therapy.

The long term side effects of using bladder drainage can have a big impact on quality of life. Many of these patients have to have surgery to change from bladder drainage to enteric drainage. Studies that have compared the outcomes of pancreas transplant using enteric drainage versus bladder drainage have found that there isn't a statistically significant difference in the two methods for graft survival, especially after 1996 with the advent of better anti-rejection meds. Long term, the digestive enzymes being drained through the bladder and urinary tract cause a long list of problems. Since 1996, with the advances in anti-rejection meds, many institutions moved away from bladder drainage altogether. I read an interesting paper in which a new approach of drainage from the donor duodenum through the recipient duodenum is being tried with good results.