 Today is the 1-year anniversary of the Renal Fellow Network. I started it towards the end of my 1st (clinical) year of nephrology fellowhip on April 23, 2008…and since this is the 320th post, I’ve done a reasonably good job at posting on a near-daily basis.
Today is the 1-year anniversary of the Renal Fellow Network. I started it towards the end of my 1st (clinical) year of nephrology fellowhip on April 23, 2008…and since this is the 320th post, I’ve done a reasonably good job at posting on a near-daily basis.
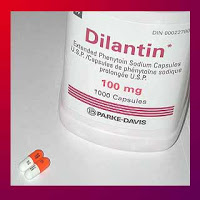
Today’s brief topic: the renal pharmacokinetics of phenytoin (Dilantin). Why this topic? It was the subject of a test question on the in-service exam and I realized I had never learned this before. This common antiepileptic drug, related to barbituates in chemical structure, is primarily metabolized in the liver. However, after the metabolites are secreted in the bile and reabsorbed in the gut, they are ultimately excreted in the urine. This occurs by two mechanisms, both via glomerular filtration, and to a large degree by tubular secretion.
Based on metabolism by the p450 system, a number of drugs (common to ESRD patients) can dramatically influence phenytoin levels, which is important to monitor given the narrow therapeutic window of the drug.
Phenytoin can be removed by dialysis in emergency situations (e.g., a massive overdose, for instance). Since phenytoin is removed by dialysis ESRD patients should be dosed following dialysis on these days. Some common drugs which increase phenytoin levels include amiodarone, salicylates, sulfonamides, and cimetidine. Others which decrease phenytoin levels include chronic alcohol use, sucralfate,and carbamazepine. In addition, oral calcium supplements should be staggered with Dilantin intake, otherwise there may be GI absorption problems of the medication.
There is a recommended “renal dosing” of Dilantin but the formula given appears to include as variables a measured phenytoin level and also serum albumin concentration–there is no inclusion of creatinine.


Are you sure that phenytoin is dailyzable and need post dialysis dose???!!!!
Kindly share with me your reference.
And how would you calculate this post dialysis dose
I cannot believe that despite a JAMA article that is easily found with Google that a fellow would make statement phenytoin is dialyzable and the emergency situations described use charcoal hemofiltration… absolutely incredulous~!
Probably most important, phenytoin is highly protein-bound. In the setting of hypoalbuminemia, therefore, less phenytoin is bound and more is “free.” Since the “free” drug is what produces the effect, this free:bound ratio is exceedingly important both for efficacy and for toxicity. If you try to increase the phenytoin dose until you hit a therapeutic TOTAL phenytoin level, you risk toxicity in a hypoalbuminemic patient. So, it is important to monitor FREE levels of phenytoin in this situation, or use the equations you cite to estimate the free level based on one’s albumin.