 I would like to direct your attention to a landmark paper in transplantation just published on the NEJM two weeks ago.
I would like to direct your attention to a landmark paper in transplantation just published on the NEJM two weeks ago.
We have previously discussed the terms used to characterize sensitized patients and the most common protocols to overcome this barrier to transplantation. Briefly, more than 30% of patients on the waiting list for a kidney transplant are sensitized to HLA antibodies, with more than 8,000 patients being highly sensitized. Sensitized patients have 3 options to undergo kidney tx:
– stay on the waiting list (hoping to get a matched kidney – annual transplantation is below 7%);
– enroll in a paired kidney donation (improves chances but still low rate); or
– undergo a desensitization protocol.
Desensitization usually involves plasmapheresis, IVIg and high dose immunosuppressive drugs (+/- rituximab) in order to decrease circulating anti-HLA antibodies. These patients have a high risk of complications, including bleeding, cancer, infection and antibody-mediated rejection (which is associated with poor allograft function). Moreover, these patients are very expensive to the hospital’s transplant program. More recently, with the spread of quality of measures in transplantation, having many sensitized patients on a program can significantly reduce the successful statistical outcomes of transplantation and consequently deteriorate the image of the program. Therefore, many programs just avoid taking highly sensitized patients.
Despite all the potential complications, whether undergoing desensitization leads to significant long-term survival benefit is unknown. Montgomery et al. analyzed a single-center cohort of 211 sensitized patients who underwent desensitization (IVIg+plasmapheresis) followed by renal transplantation, comparing with two carefully matched control groups of patients on a waiting list for kidney tx who continued to undergo dialysis (dialysis-only group) or who underwent either dialysis or HLA-compatible transplantation (dialysis-or-transplantation group). During the 11-year study period, 98% of the sensitized patients underwent successful transplantation and this study included patients with different detection methods of anti-HLA antibodies, such as positive cross-match by cytotoxicity assay, flow cytometry and/or bead assay (Luminex).
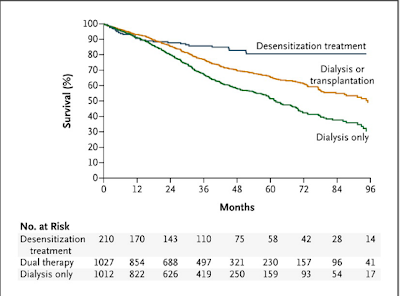
In the desensitized group, rates of survival were 90.6% at 1 year, 85.7% at 3 years and 80.6% at 8 years, compared with 91.1%, 67.2% and 30.5% in the dialysis-only group (view figure). Among the different levels of anti-HLA antibodies, patients with positive cross-match by cytotoxicity assay carried the worst outcome. Nonetheless, the survival benefit curve crossed at 18 months even in that group. Combining all sensitized groups, the survival benefit was clear after 12 months.
Overall, major adverse events during desensitization treatment occurred in less than 5% of patients, including anaphylaxis or bleeding. The most common cause of death was cardiovascular disease (~16% patients) and there were 6 deaths related to infection (~3%), which were likely secondary to the intensive immunosuppression produced by the desensitization protocol. In summary, sensitized patients can obtain a significant survival benefit by undergoing desensitization followed by kidney transplantation compared to alternative options, but risks of infection are higher and more studies are needed to help identify patients at greatest risk of dying and suffering from complications like malignancy or cardiovascular disease.

Those are very good points Martina and I do think they could have given more details about the transplant/dialysis group. I think the graft survival omission was on purpose to focus the manuscript on survival. Specially since the ultimate goal of transplantation is to improve survival and NEJM is a general medicine journal. My guess is that they will publish another paper with the graft survival curves for the three different anti-HLA positive groups (disappointing for us transplant nephrologists though…). Regarding levels of sensitization, the PRA is not as important as the level of anti-donor antibody. Patients that have anti-donor HLA antibodies higher than 1:32 dilution are much harder to get desensitized and sometimes unable to undergo desensitization. As we used novel drugs like rituximab in the desensitization protocol, this could be a moving point.
Nice post Leo. Are any patients you would consider "too sensitized" for desensitization? For example, people with 100% PRA or very high Ab titers?
Interesting study that addresses an important question. Two things surprise me though- one, there's no information on the number/proportion of patients within the dialysis/transplantation group that actually got a kidney, so its hard to know what they truly represent as a control group; and secondly, why is there no data on graft survival? These issues are particularly relevant for the CDC positive group as the survival curves didn't cross until 30 months