CMV infection still remains one of the most common and unpredictable complications in transplant recipients, and the negative consequences in terms of graft lost and recipient survival are well known. In this setting, I would like to present a remarkable kidney transplant case from our institution: an unsensitized 40 y/o female, IgG seropositive for CMV was transplanted from a seropositive deceased donor. She had taken the standard immunosuppressive therapy, and after 2 months was diagnosed with CMV-disease. Considering the situation above, one may question why this happened and how could it have been possible to predict this outcome.
 Currently, the immune-risk stratification before transplant is based only on CMV-specific antibody (IgG+) of donor and recipient. However, the cellular immunity is crucial in controlling the viral replication and conferring long-lasting protection. The proportion of both CD4+ and CD8+ T cells committed to the anti Human CMV (HCMV) response is large, ranging from 10 to 40% in peripheral blood.
Currently, the immune-risk stratification before transplant is based only on CMV-specific antibody (IgG+) of donor and recipient. However, the cellular immunity is crucial in controlling the viral replication and conferring long-lasting protection. The proportion of both CD4+ and CD8+ T cells committed to the anti Human CMV (HCMV) response is large, ranging from 10 to 40% in peripheral blood.
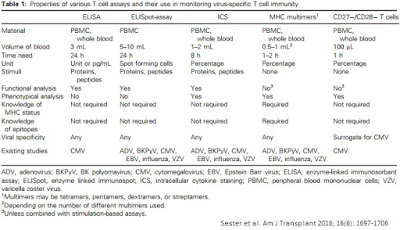
In this scenario, novel immune assays may play a mainstay role. They consist in evaluating physiological response of HCMV specific T cells (cell activation, cytokine expression or proliferation) through antigen stimulation in vitro (virus-infected cells lysates or virus-like particles). As depicted in Table 1, these tests have different characteristics; therefore a physician must know how to choose the best test for a specific situation.
Similar cases have already been described and one may conclude that these patients lack cellular-immunity. On the other hand, seronegative recipients who have low rate of specific T cell have also been described. In this scenario, these new tests could give information on how to predict the ability to control viral replication. Hence, T cells analysis can justify a whole new perspective of prophylaxis indications.
Also, in posttransplant situations (Figure 1), serial evaluation of viral load and T cell test are important to guide therapy and foresee relapse after its cessation.
 Low levels of CMV-specific T cell response correlates well with reactivation of CMV-infection and late-onset disease; immediate treatment or prolonged prophylaxis would hold back these outcomes. Therefore, an individualized approach with measurement of CMV specific cellular and antibody response will be crucial in the improvement of transplant outcomes, in particular in centers that do not routinely use CMV prophylaxis.
Low levels of CMV-specific T cell response correlates well with reactivation of CMV-infection and late-onset disease; immediate treatment or prolonged prophylaxis would hold back these outcomes. Therefore, an individualized approach with measurement of CMV specific cellular and antibody response will be crucial in the improvement of transplant outcomes, in particular in centers that do not routinely use CMV prophylaxis.
Abel Portela
References:
Kotton CN, Kumar D, Caliendo AM et al. Updated International ConsensusGuidelines on the management of cytomegalovirus in solid-organ transplation.Transplantation 2013; 96: 333-360.
