The landscape of Primary Membranous Nephropathy (PMN) has significantly
changed over the last decade. Most of what we now understand about the
pathogenesis of PMN is derived from the Heymann Nephritis model in rats. In
1959, Dr. Walter Heymann published this landmark article,
which established the autoimmune nature of the disease. In the late 1970s, two
groups (Dr. Couser et al
in Boston and Dr. Van Damme et al
in the Netherlands) established that the deposits of Heymann Nephritis were not
from circulating immune complex trapping, but due to in situ formation. The rat antigen was eventually identified as megalin.
The human antigen equivalent remained unknown until much later. Finally, 2009, Salant,
Beck et al found that 70% of adult patients with “idiopathic”
membranous nephropathy had antibodies against M-type phospholipase A2 receptor
(PLA2R), a transmembrane glycoprotein found on podocytes. Soon after, another
podocyte transmembrane glycoprotein called thrombospondin type-1
domain-containing 7A (THSD7A) was discovered (See NEJM 2014;
371(24):2277-2287).
changed over the last decade. Most of what we now understand about the
pathogenesis of PMN is derived from the Heymann Nephritis model in rats. In
1959, Dr. Walter Heymann published this landmark article,
which established the autoimmune nature of the disease. In the late 1970s, two
groups (Dr. Couser et al
in Boston and Dr. Van Damme et al
in the Netherlands) established that the deposits of Heymann Nephritis were not
from circulating immune complex trapping, but due to in situ formation. The rat antigen was eventually identified as megalin.
The human antigen equivalent remained unknown until much later. Finally, 2009, Salant,
Beck et al found that 70% of adult patients with “idiopathic”
membranous nephropathy had antibodies against M-type phospholipase A2 receptor
(PLA2R), a transmembrane glycoprotein found on podocytes. Soon after, another
podocyte transmembrane glycoprotein called thrombospondin type-1
domain-containing 7A (THSD7A) was discovered (See NEJM 2014;
371(24):2277-2287).
Now, approximately 85% of PMN is found to be mediated by
anti-PLA2R or anti-THSD7A, with still 15% of PMN “idiopathic”. With a serologic
test for anti-PLA2R now commercially available as well as a biopsy
immunofluorescent stain, the diagnosis and management of patients with PMN has
been completely revamped.
anti-PLA2R or anti-THSD7A, with still 15% of PMN “idiopathic”. With a serologic
test for anti-PLA2R now commercially available as well as a biopsy
immunofluorescent stain, the diagnosis and management of patients with PMN has
been completely revamped.
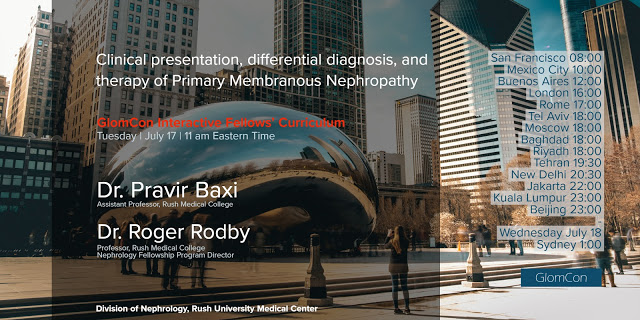
For more on this discussion, please join us in the next GlomCon
Interactive Fellows’ Curriculum on Tuesday,
July 17th at 11 am eastern time. We will be walking through a case scenario
as we review several different aspects of PMN.
Interactive Fellows’ Curriculum on Tuesday,
July 17th at 11 am eastern time. We will be walking through a case scenario
as we review several different aspects of PMN.
To join the meeting go to: https://glomcon.zoom.us/ and select
‘Join a Meeting’. Enter the Meeting ID into the web site (or connect directly
from your Zoom app).
‘Join a Meeting’. Enter the Meeting ID into the web site (or connect directly
from your Zoom app).
Meeting ID: 394-801-817
You HAVE to be logged into ZOOM to join the session. You may
either create a free ZOOM account, or sign in through a Google or Facebook
account (if you have one).
either create a free ZOOM account, or sign in through a Google or Facebook
account (if you have one).
Alternatively, use your institution’s ‘Polycom’ system,
enter IP address:
enter IP address:
US West: 162.255.37.11
US East: 162.255.36.11
Europe: 213.19.144.110
Then, enter the Meeting ID: 394-801-817