Fibrillary glomerulonephritis (GN) is a rare disease which accounts for about 1% of all kidney biopsies. The very first description of the disease was published by Rosenmann and Eliakim in 1977. They described a patient with nephrotic syndrome due to deposition of what they describe as “an amyloid-like material in the glomeruli,” but upon ultrastructural analysis, this material “appeared shorter than amyloid fibrils”
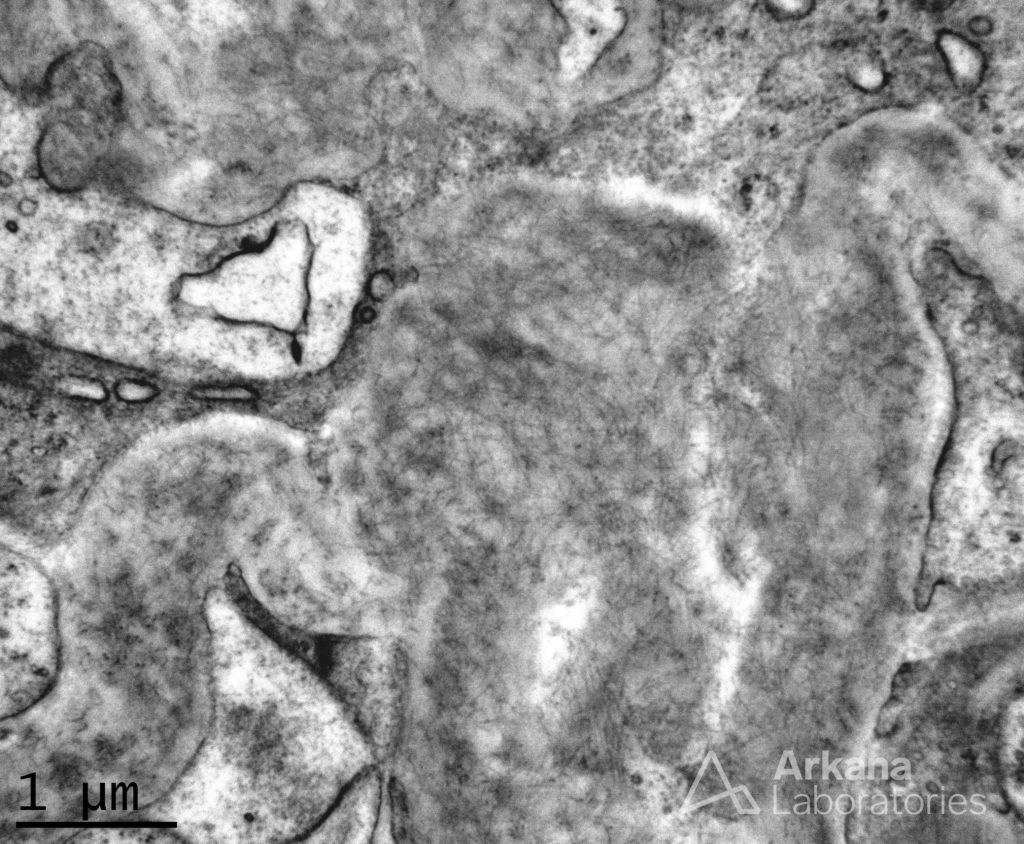
In 1983, Duffy et al identified this entity as “renal fibrillosis” and described 8 such patients presenting with hematuria, proteinuria, hypertension, and reduced kidney function. The deposits stained negative with Congo-red or Thioflavin T, and by electron microscopy revealed fibrils (Figure 1) which “resembled amyloid fibrils in their location but wider than amyloid (20 nm) and up to 1500 nm in length”. Interestingly, Congo-red positive fibrillary GN has also been described.
More than four decades since the first description of this disease entity, the diagnosis of fibrillary GN remains a challenge. Much of the difficulty in diagnosis has been attributed to the histological polymorphism of the disease (Table 1).
Table 1. Fibrillary GN Histological Findings (LM: light microscopy; IF: immunofluorescence; EM: electron microscopy)
Recently, researchers have determined that a novel protein, DNAJB9, may be the missing link to diagnose this elusive disease.
What is DNAJB9 – (DNAJ homolog subfamily B member 9) and how does it help us?
DNAJB9 belongs to a family of proteins that function as “co-chaperones” to heat-shock protein 70 (hsp-70). It is expressed in all healthy tissues and is localised to endoplasmic reticulum (ER) and is upregulated by ER stress, nitric oxide, and other inflammatory mediators. Lee et al demonstrated that DNAJB9 is induced by p53 and this is primarily mediated through Ras/Raf/ERK pathway. DNAJB9 in turn inhibits the pro-apoptotic function of p53 through its J-domain (AA 93), that is a conserved 70 AA sequence found in proteins belonging to DNAJ family. Dasari S et al from the Mayo Clinic analysed the protein content of glomeruli in patients affected by fibrillary GN and discovered DNAJB9 as the fourth most abundant molecule in this group. However, it was absent in the glomeruli of patients with amyloidosis, non-fibrillary GN glomerular disease, and a healthy subcohort.
Interestingly, the DNAJB9 molecule deposited in the glomerulus had no structural or sequence alterations as analyzed by Sanger sequencing – so it is the “normal DNAJB9” that accumulates in fibrillary GN. The underlying reason for DNAJB9 deposition is unknown, but may be related to exaggeration of its physiological role as a stress molecule. Another very intriguing fact is that DNAJB9 has been demonstrated to co-localize with IgG and is seen as smudgy deposition on IHC – in a manner similar to IgG; probably suggesting that DNAJB9 is indeed a content of fibrils.
DNAJB9 can be demonstrated in fibrillary GN by mass spectrometry – the same method which is employed for typing of amyloid fibrils. It can also be demonstrated by immunofluorescence (IF) or immunohistochemistry (IHC). Since we know that DNAJB9 is expressed in all healthy tissues, it is important to note that there may be weak background staining in normal tissues as well, but it is “homogenous smudgy intense extracellular staining” in the mesangium and glomerular capillary wall which characterises the pattern in fibrillary GN. Since fibrillary GN is a great masquerader even ultrastructurally, DNAJB9 IHC/IF could very well replace EM in the near future if fibrillary GN is suspected. Currently, DNAJB9 testing is available routinely in only a few specialized laboratories, but given its utility, its use may become more widespread.
An interesting deduction can be made with respect to the therapeutic aspect of this discovery. Since the induction of DNAJB9 by p53 is mediated through Ras/Raf/ERK pathway, inhibitors of the pathway like sorafenib could theoretically, be beneficial for the treatment. This theory needs to be confirmed with clinical trials (which are hard to conduct given that this is a rare disease). Needless to say, whether DNAJB9 is a mediator of kidney damage in fibrillary GN, or an innocent bystander is also not clearly established yet.
To conclude, the recently identified specificity of DNAJB9 for fibrillary GN can be considered one of the ground-breaking discoveries in nephrology. With a sensitivity of 98 –100% and specificity of 99–100%, DNAJB9 is a promising biomarker which will simplify the diagnosis of an elusive disease.
Post by: Lovy Gaur
NSMC Intern, 2019


Really very informative. Thank you.
Good going Dr. Lovy! Very informative..