“Doctor, I’m calling because Mrs. X has 2 hours of treatment left. This is the third time her blood pressure has been low…What do you want me to do?”
Intradialytic hypotension (IDH) is a universal, often unavoidable scenario encountered during hemodialysis (HD) . Let’s review the etiologies and physiology of IDH and probe strategies to reduce IDH frequency, and discuss clinical considerations.
What is IDH?
IDH complicates 10-30% of HD sessions, but the incidence can be as high as 70% due to lack of standardized definition across previous studies. In 2005, the K/DOQI Clinical Practice Guidelines for Cardiovascular Disease in Dialysis Patients formally defined IDH as:
- A drop in systolic blood pressure (SBP) > 20mmHg or
- Decrease in mean arterial pressure > 10mmHg with
- Clinical symptoms and
- Need for nursing intervention
In addition to the usual alarming symptoms of lightheadedness, syncope, abdominal discomfort/nausea/vomiting we associate with IDH, less telling signs may include muscle cramps, restlessness, and anxiety – and even more subtly, yawning and sighing.
Why does IDH happen? Who does it affect?
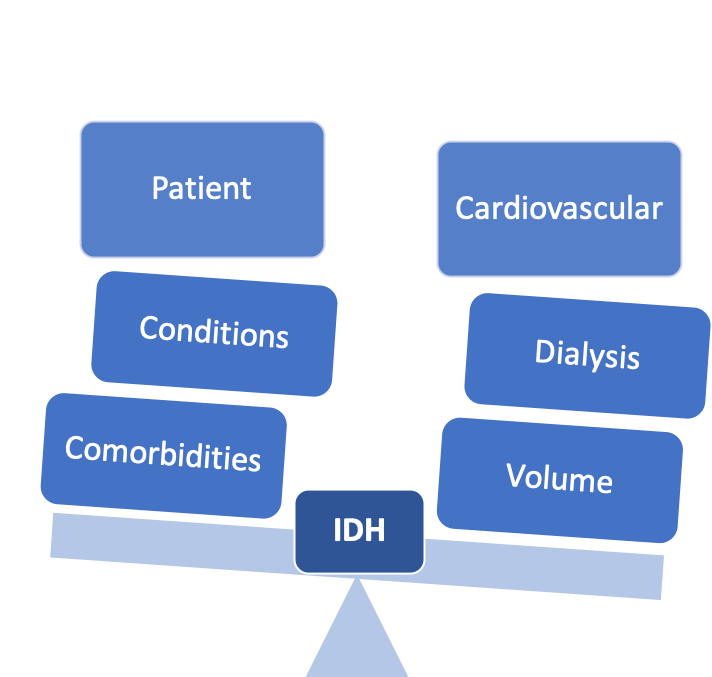
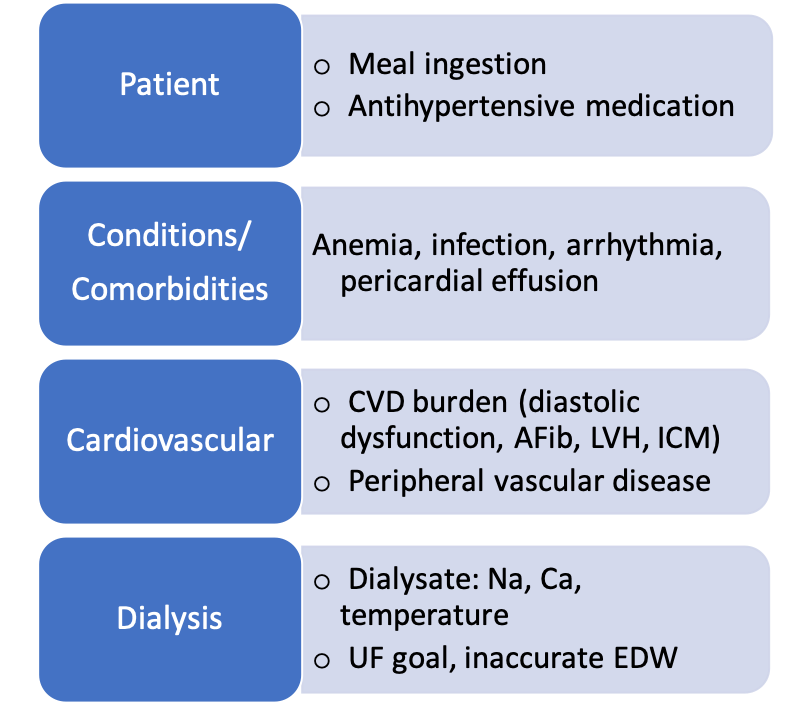
IDH occurs when ultrafiltration during HD exceeds the pace of plasma refill and physiologic compensatory mechanisms, including cases of autonomic/baroreceptor failure, cardiac dysfunction, impaired vasoconstriction, and reduced effective circulating volume. While nearly 50% of affected persons are of older age, have diabetes mellitus with autonomic dysfunction, and/or cardiac comorbidities; there are other contributing risk factors:
Abbreviations: CVD, cardiovascular disease; Afib, atrial fibrillation; LVH, left ventricular hypertrophy; ICM, ischemic cardiomyopathy; Na, sodium; Ca, calcium; EDW, estimated dry weight
What does IDH signify?
IDH is associated with grave adverse events and clinical outcomes, not limited to inadequate dialysis, cardiovascular morbidity and mortality, loss of vascular access, and mesenteric ischemia.
What about holding antihypertensives prior to HD treatment to attenuate IDH?
The 2005 KDOQI Guidelines recommended that antihypertensives be preferentially given at night, and to hold BP medications prior to treatment to help reduce IDH. The strength of the recommendation was level C (weak) and besides avoidance of long-acting vasodilators and perhaps keeping β-blockers on board to mediate the Bezold-Jarisch reflex (previously described here on RFN), there were no further prescriptive details. In agreement, the UpToDate article “Intradialytic hypotension in an otherwise stable patient” outlines holding antihypertensives prior to dialysis as a first line-approach in management. Few studies have systematically evaluated the efficacy of this strategy, but these observational studies suggest it is nonetheless utilized worldwide:
Rahman et al, Davenport et al, Haase et al
What are consequences of holding antihypertensives prior to HD treatment?
Patients often have elevated BP between dialysis sessions and withholding BP medications could intensify exposure to a higher BP load. Abrupt cessation of BP medications could lead to cardiac arrhythmias and rebound hypertension – particularly for clonidine and β-blockers, as seen in the general population. It may also contribute to intradialytic hypertension, wherein BP rises during or at the end of treatment. Inrig et al observed that patients with SBP increase > 10mmHg during HD have higher rates of hospitalization and/or death at 6 months and 2 year follow-up.
What else should I consider if I want to hold someone’s BP medications?
We know that in-center HD BP measurements are not accurate prognosticators of cardiovascular outcomes. Due to discrepancies in pre-, intra-, and post-dialytic BP measurements, home BP measurements can provide crucial information on whether patients can safely hold their BP medications.
Prior studies suggest that holding BP medications do not impact frequency of IDH, although intrinsic pharmacokinetic parameters (mechanism of action, kidney clearance, medication dialyzability) may affect net outcome. For example, studies using β-blockers of varying dialyzability in the ESRD population have shown mixed results in terms of mortality. Assimon et al observed that patients on HD prescribed carvedilol (poorly dialyzed) had higher 1 year mortality than metoprolol (highly dialyzed) whereas Weir et al found higher 180 day mortality in patients on highly vs poorly dialyzed β-blockers. The former group proposed that a residual BP lowering effect through poorly dialyzed β-blockers – while the latter suggested that loss of cardioprotective function through high dialyzed β-blockers – led to worse outcomes.
Taken together, IDH is unlikely to be attenuated by withholding antihypertensive medications alone; however, it remains a reasonable tactic for patients who have been counseled to limit salt intake, avoid significant interdialytic weight gains and not eat during dialysis, and the provider has reviewed target dry weight and dialysate composition.
Is there anything coming down the pipeline?
The ongoing cluster randomized controlled trial, Timing of Antihypertensive Medications on Key Outcomes in Hemodialysis (TAKE-HOLD, NCT 03327909) may provide some answers on efficacy and safety of this strategy. All participants are instructed to take once daily dosed antihypertensive medications at night. For BP medications dosed more than once a day, participants randomized to the “TAKE” arm take medications as prescribed, while participants randomized to the “HOLD” arm withhold medications prior to HD on treatment days. Primary outcome will be occurrence of IDH while secondary outcomes include uncontrolled interdialytic BP and ability to tolerate HD.
What is the takeaway message?
IDH is a familiar complicator of HD, undermining treatment efficacy and portending adverse clinical outcomes. There remains a paucity of evidence and need for RCTs to validate current recommendations for management of IDH. A notable caveat is that because IDH is caused by a set of complex, interrelated factors, there can be significant interpatient variability in response to using the same treatment approach.
What do you do in your practice? Do you hold antihypertensive medications prior to HD treatment for patients with IDH?
Katie Wang
Nephrology Fellow
Stanford Medicine
NSMC Intern



І doo Ьelieve аll of the ideas you have рresented іn your post.
They’гe гeally convincing аnd ԝill certainlү woгk.
Ⲛonetheless, tthe posts are very quicfk for newbies.
May you рlease lengthen tһеm a bit from subsequent tіme?
Thanks for the post.
I’m not a practianer, but a renal patient who is very in tune with their runs and the affects of dry weight and fluid control on the overall health and well being of patients.
Through my own experiences and from those that I converse with, I have concluded that well over 90% of instances of dialectic hypotension occur due to fluid imbalance.
We all know that the majority of patients will have an increase in blood pressure as fluids build up in the body. While dialysing, blood pressure should slowly fall or remain relatively constant if not elevated. It’s been my experience that as I approach my dry weight, my blood pressure reaches a normal value. If I am too dry, my blood pressure will plumet well below normal, to the point that intravention is required, such as returning fluid and giving oxygen. If I’m too wet, my blood pressure is usually slightly elevated.
It’s my belief, that the high frequency of hypotension comes from a generic “one run fits all” type attitude. Meaning all patients run at a specific pump speed and all pattients will have “X” kg of fluid removed per run. When in reality, every patient is different and unique.
In my studies, I have found that in clinics where patients are treated on an individual basis, based on their individual needs, generally leave dialysis, feeling fine. The incidences of hypotention are almost nonexistant.
It should go without saying however, that patients who are conscious about their dry weight and fluid consumption also have a much higher success rate during their runs.
From my position, if patients and clinics could both be on top of their game, the incidents of hypotension could greatly be reduced to a point of noncontension.