Peritoneal dialysis (PD) treatment began much earlier than hemodialysis but was not successful due to the many complications associated with it and the difficulties with access to the peritoneal cavity. It was in 1946 that Dr. Fine and his colleagues from Beth Israel Hospital in Boston described methods for their successful cases of continuous peritoneal irrigation in patients with acute renal failure. In 1968, Tenckhoff and Schechter designed the permanent PD catheter with silicone tube and polyester cuffs, making PD as an acceptable alternative for long term therapy for renal failure.
So, how do we define adequacy in PD?
NKF KDOQI guidelines from 2006 recommend targeting a Kt/V (urea) of at least 1.7 in peritoneal dialysis patients.
We also know that residual renal function is important. In this post, we will briefly summarize important studies that helped us reach these conclusions. Check out this 2018 #NephMadness post from the #PeritonealDialysis Region (and a couple #NephMadness visual abstracts below).
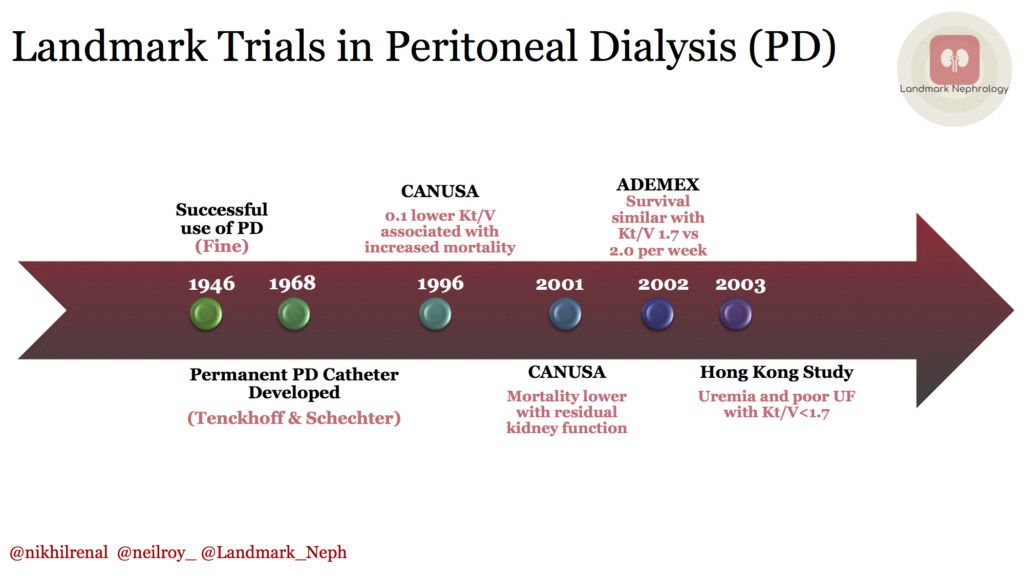
1. CANUSA (1996)
680 patients initiating PD between 1990 and 1992 at 14 centers in US and Canada were enrolled. 97.9% were on CAPD (manual) and dialysis prescription was prescribed by the individual patient’s physician. Adequacy of dialysis was estimated by measurement of total weekly Kt/V for urea, total weekly creatinine clearance (CCr). The findings were remarkable. A 0.1 lower Kt/V was associated with 6% increase in the RR of death and 5 L/wk lower CCr, associated with 7% increase in the RR of death. For weekly Kt/V of 2.3, 2.1, 1.9, 1.7, and 1.5, expected 2-yr survivals were 81%, 78%, 74%, 71%, and 66% respectively.
The study concluded that it would appear reasonable to provide as high a dialysis dose as is feasible with a Kt/V of 2. 1 or a CCr of 70 L/week.

But….it assumed that peritoneal dialysis clearances and residual renal function clearances are equivalent. That led to…
1a. CANUSA (Re-analysis, 2001)
CANUSA data was reanalyzed to address the assumption that renal and peritoneal clearances are comparable and therefore additive. The findings were again remarkable. A 5-L greater weekly GFR was associated with a 12% decrease in the RR of death
But…It found no association between the same increase in peritoneal creatinine clearance and the RR of death. In fact, for each increase of 250 ml of urine per day, there was a 36% decrease in the RR of death. Thus reflecting the importance of residual renal function, and questioning the utility of targeting higher Kt/V.
2. ADEquacy of PD in MEXico, ADEMEX (2002)
This was a randomized control trial (RCT) which enrolled 965 patients in 1998-1999 and followed them for 2 years with death as the primary end point. The control group received 4 daily exchanges of 2 L vs the intervention group which received multiple 2.5L to 3L exchanges to achieve a peritoneal creatinine clearance (pCrCl) value of 60 L/wk per 1.73 m2. It essentially compared 47 vs 60 L/wk/1.73 m2 of creatinine clearance or Kt/V of approximately 1.7 vs 2.0 per week. Importantly, residual renal function was similar in 2 groups.
They found that patient survival was similar for the control and intervention groups. Age, diabetes mellitus, serum albumin levels, residual renal function were all identified as significant factors associated with patient survival.

Lastly, this RCT enrolled 320 new CAPD patients across 6 centers in Hong Kong with baseline renal Kt/V < 1.0, mean follow up period was 24.3 months. They were randomized to three Kt/V targets:
Group A: 1.5 to 1.7; Group B: 1.7 to 2.0; Group C: >2.0
They found that the total Kt/V did not significantly affect survival. There was also no difference in serum albumin, composite nutritional index (CNI) scores, and hospitalization rate. However, in Group A, a significantly higher number of patients were withdrawn from the study mainly due to inadequate ultrafiltration and clinical inadequacy of dialysis and more group A patients required EPO, possibly suggestive of uremia.
Post by: Nikhil Agrawal, MD and Neil Roy, MD
Landmark Nephrology is an online learning tool designed to collect landmark trials in nephrology and distribute content that makes learning nephrology fun and easy.
Please visit us to check out our topic-specific content including videos, visual abstracts, quizzes, and a new slide-share portal to facilitate the exchange of educational material within the nephrology community.
We love collaboration so contact us as landmarknephrology@gmail.com or find us on Twitter to get involved!


