Apical window is a component of the standard FoCUS examination and is mainly used for the assessment of right ventricular systolic function, and its size relative to the left ventricle. It is also best for the Doppler interrogation of mitral and tricuspid valves. In addition, this window is helpful for evaluation of left ventricular regional wall motion abnormalities and differentiate circumferential vs localized pericardial effusions. There are various apical views such as the four-chamber, five-chamber, two-chamber, long-axis and short-axis that can be obtained from this window, but the two frequently used views for focused exams are the four-and five-chamber.
How are the images acquired?
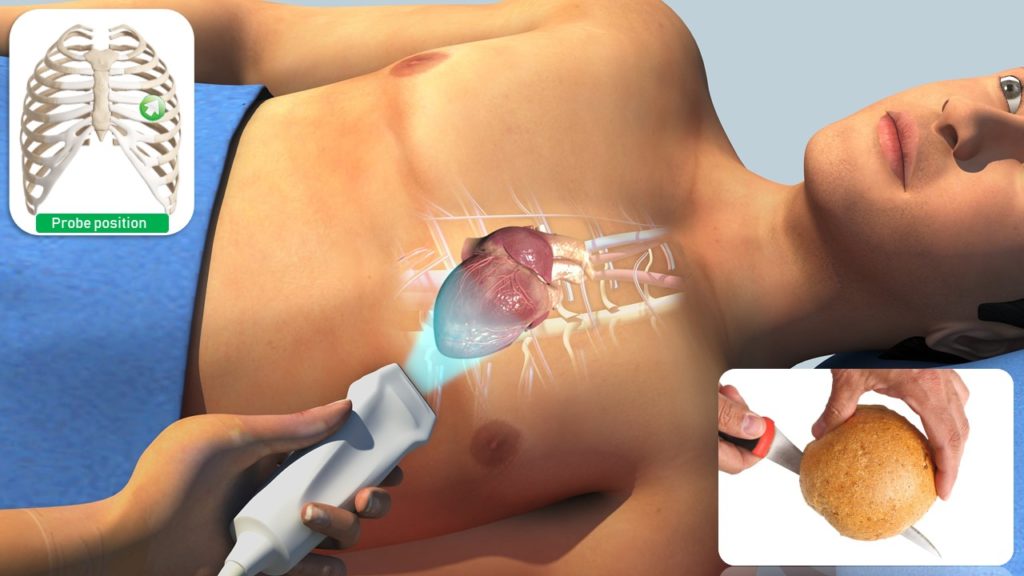
Acquiring adequate quality images from the apical window can be challenging and requires more practice than that of parasternal and subcostal views. Whenever possible, positioning the patient in the left lateral decubitus position helps. Apical four-chamber view is obtained by placing the transducer in the 4th or 5th intercostal space with orientation marker facing the patient’s left shoulder (somewhere between 2 o’ clock and 3 o’ clock position works for most patients). More practical way is to identify the apical impulse and placing the transducer there. Tilt the face of the transducer towards the head of the patient till the four chambers come into view. The transducer should be then gently swept to align the interventricular septum in a vertical position in the center of the screen. The ultrasound beam slices the heart similar to cutting a bread roll in half [Figure 1].
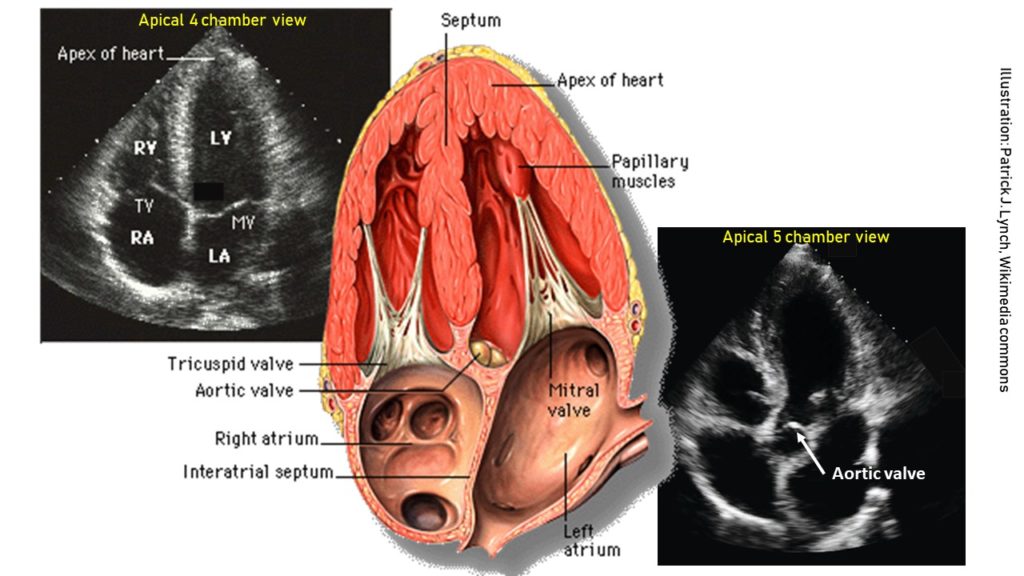
From the four-chamber view, if the probe is tilted slightly upwards, the aortic valve and the left ventricular outflow tract appear. This is called the apical five-chamber view (5th chamber being the left ventricular outflow tract) and is helpful to assess the aortic valve function [Figure 2].
Sonographic anatomy and orientation:
The four-chamber view [Figure 3] demonstrates all four chambers of the heart that is, two atria and two ventricles. The ventricles are on the top of the image as we are imaging from the apex of the heart and structures closer to the probe are displayed at the top of the image as discussed before. As the probe marker is pointing to the left shoulder, the image toward the screen orientation indicator corresponds to left side of the heart and the opposite, right. The left ventricle appears as a truncated ellipse with a longer length than width and a tapered but rounded apex. The right ventricle is triangular in shape with a cavity up to two-thirds of the left ventricle. This is important to remember when looking for a dilated right ventricle. If you want to obtain precise measurements, a right ventricular diameter of >41 mm at the base and >35mm at the mid-level is considered abnormal. In addition, the right ventricle is more trabeculated and its apex is less round and more basal than the left ventricle. Also note that the tricuspid annulus lies slightly (up to 1.0 cm) closer to the apex than the mitral annulus. The five-chamber view [Figure 4] is similar to the four-chamber view except that the aortic valve and the left ventricular outflow tract are seen. This is a great view for the Doppler interrogation of the aortic valve as the flow through it is almost parallel to the ultrasound beam (ideal Doppler angle).
Tips for image optimization:
In a good apical four-chamber view, all four chambers are visualized and the interventricular septum is vertical in the center of the image. Below are the three common types of suboptimal images, which can be corrected by appropriate probe positioning.
- Atria not visible
If you don’t see the atria, the transducer may be aimed too posterior. Tilt the face of the transducer upwards till they completely come into view [Figure 5].
Note that the interatrial septum lies parallel to the ultrasound beam in apical four-chamber view, so “dropout” or absence of reflected signal from the region of the fossa ovalis is common. This should not be mistaken for an atrial septal defect. You can see this here in the right image (interatrial septum appears to disappear at the bottom of the image).
2. Tilted heart
If the heart appears tilted to the anatomic left, you are too medial. Moving the transducer laterally should help [Figure 6].
3. Left ventricular foreshortening:
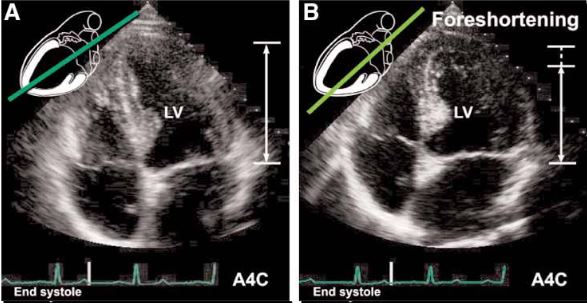
If the transducer is not positioned at the true apex, the left ventricle will appear foreshortened, with a spherical shape and little tapering of the apex instead of the normal bullet shape. Foreshortening must be distinguished from disease processes, such as chronic aortic regurgitation, which result in increased sphericity of the ventricle. On the other hand, pathologies of the apex such as infarction or a thrombus can be missed in this kind of image. This can be corrected by moving the probe more apically (1 intercostal space below) and laterally [Figure 7].
Figure 8 is another example of this phenomenon.
In the next post, will talk about some of the must-know abnormalities seen in this view.



Just awesome
Very well written article. Waiting for the next part.