Peritoneal dialysis (PD) catheters are one of the most successful long-term transcutaneous access devices ever used in medical practice. The catheter, if successfully placed can provide successful dialysis for years. For the above to be accomplished, various components of the catheter must be precisely placed in different tissues and spaces, such as the lower part of the peritoneal cavity, the rectus muscle, and the subcutaneous space. POCUS is an invaluable tool not only to guide the percutaneous placement of the catheter but also to confirm the appropriate locations and diagnose complications such as infection at the bedside. In this post, we will discuss some scenarios where POCUS can provide useful diagnostic information in PD patients.
First, it is important to understand the location of the 2-cuff, coiled tip Tenckhoff catheter (standard PD catheter). The catheter tip is in the deep pelvis away from the omentum and the exit site (typically lower abdomen, rarely chest) is chosen based on the patient’s body habitus and other special needs. The catheter has 2 cuffs: superficial cuff is subcutaneous, usually ~2 cm from the skin exit site and the deep cuff is located within the rectus muscle, near the lateral or medial border of the rectus sheath [Figure 1]
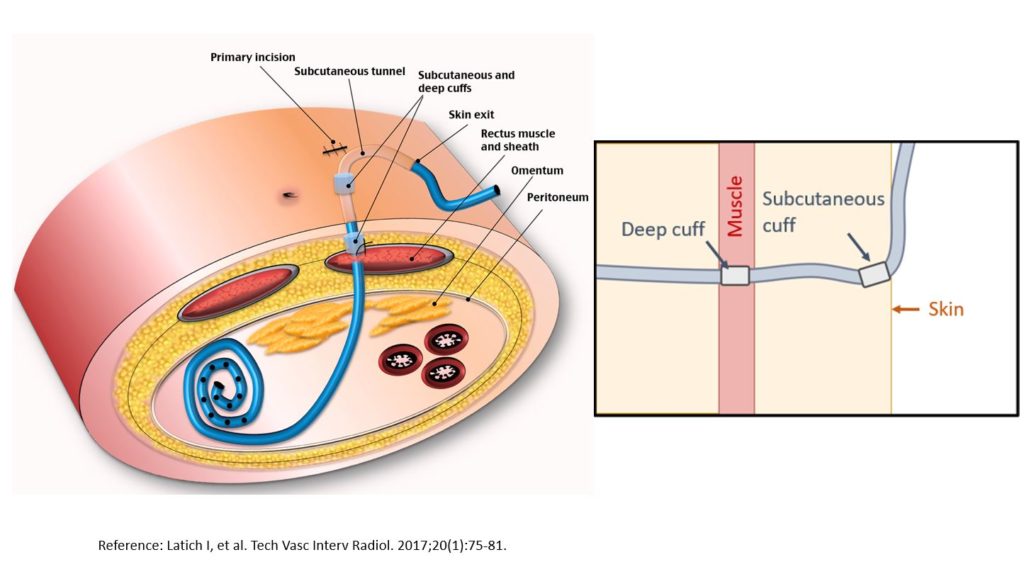
Figure 1: Schematic figure showing the abdominal wall layers with relative positions of the primary incision, skin exit site, sub-cutaneous and deep cuffs, and the catheter tunnel.
For sonographic assessment of the PD catheter, a linear (= high frequency) transducer is preferred as it provides adequate visualization of the superficial structures including the catheter. It is possible to trace the catheter all the way to its disappearance or downward dip into the rectus sheath in most individuals. This may prove tricky in obese individuals in whom catheter can course a little deeper. In such individuals, the curvilinear (= abdominal) probe can be used to visualize the catheter’s entry into the rectus sheath. A vascular preset is preferred to prevent noise from superficial structures and movement with respiration.
Here is how a normal abdominal wall ultrasound looks like [Figure 2]. Familiarity with these structures makes it easier to identify the abnormalities.
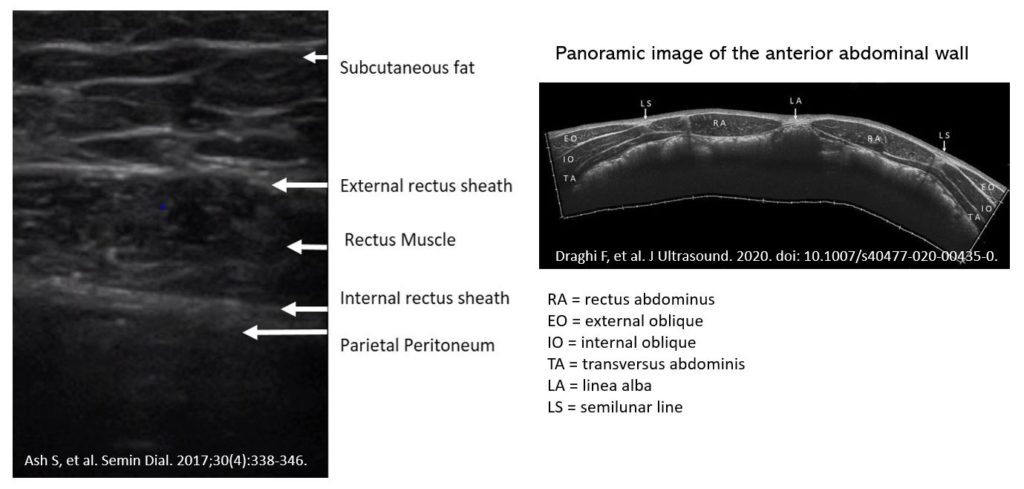
Figure 3 demonstrates the normal appearance of a PD catheter. Note the presence of 4 curved lines, depicting the inner and outer layers of the silicone catheter.
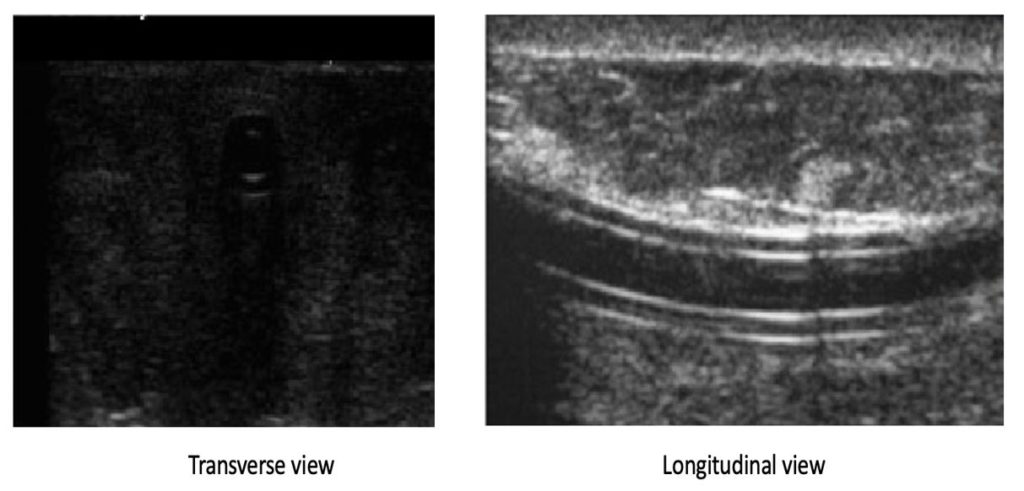
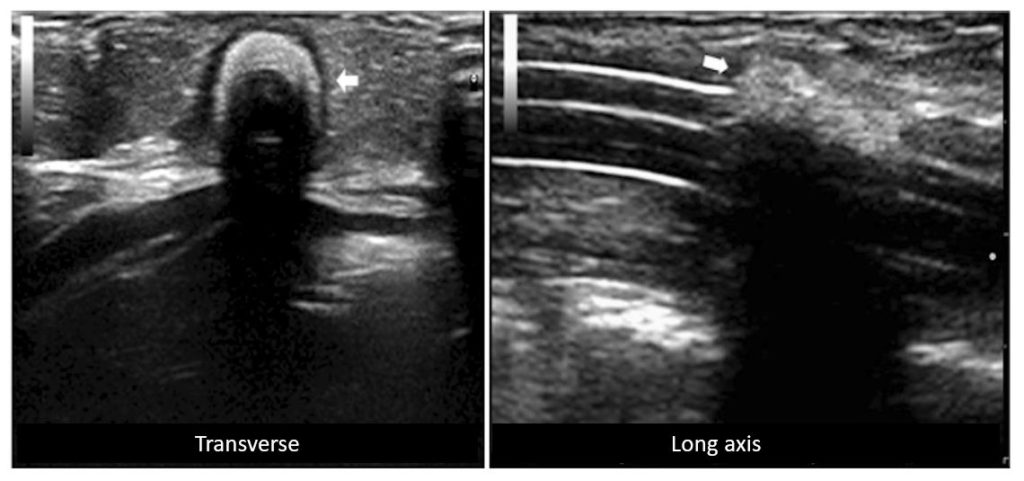
Figure 4 demonstrates another normal catheter (arrowhead) in transverse and longitudinal views, respectively. The area of hyper echogenicity noted around the catheter (arrow) is normal and is related to the normal chronic inflammatory response due to the catheter.
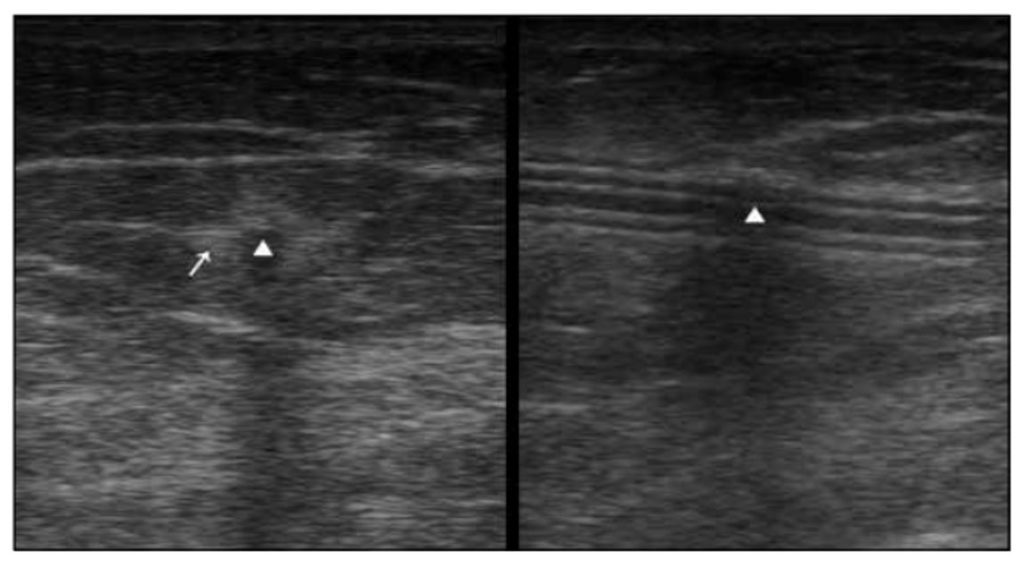
Figure 5 illustrates the normal appearance of the cuffs of a PD catheter. Left panel is the superficial cuff in the fat with normal shadowing (‘cuff shadow’) and the right panel represents the deep cuff within the rectus muscle, again with a shadow. Note that the cuff material is not clearly visible, but the presence of a well-defined shadow is a clue to identify these catheter components.
In children, the images are well-defined and crisper because of the superficial location of the catheter. Following are the high-resolution images of catheter cuff in a child obtained using linear transducer [Figure 6]. Note the hyperechoic cuff (arrows) followed by shadow.
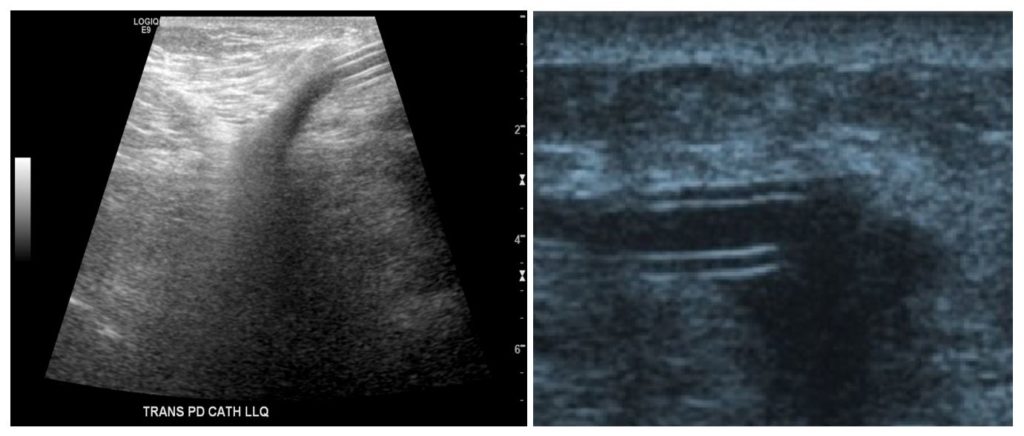
In adults, the catheter is not typically traceable all along its length. This is one of the limitations of the ultrasound in diagnosing deeper pathologies such as omental wrap or luminal obstruction. In the following images, the catheter appears to disappear at one point because it is taking a downward turn into the rectus muscle [Figure 7]. This is a normal occurrence.
Let us now look at some images of infection. In the following images [Figure 8], note the presence of a distinct hypoechoic region around the cuff, which is suggestive of infection. This is called the “signet ring” sign. Right panel shows spread of peri-catheter collection (arrow), concerning for uncontained infection.
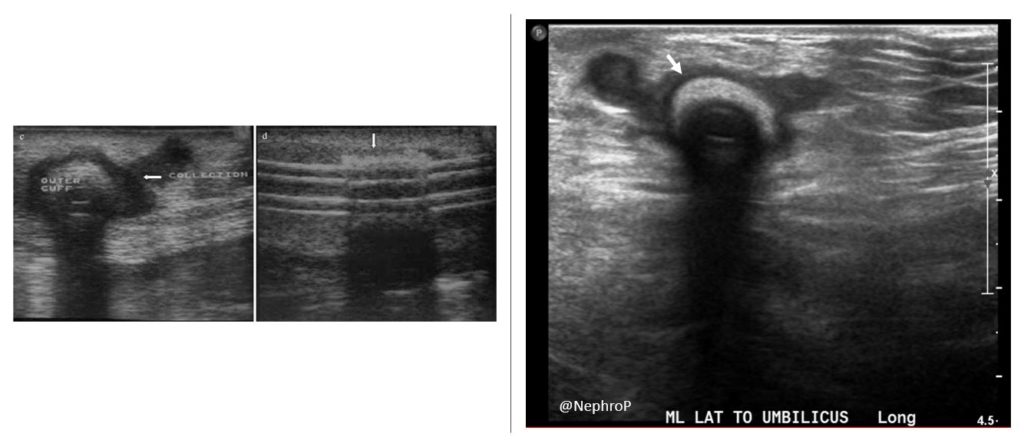
Figure 9 demonstrates two more cases of tunnel infection: Note the hypoechoic collection (asterisks) around and adjacent to the catheter (arrow/arrowhead).
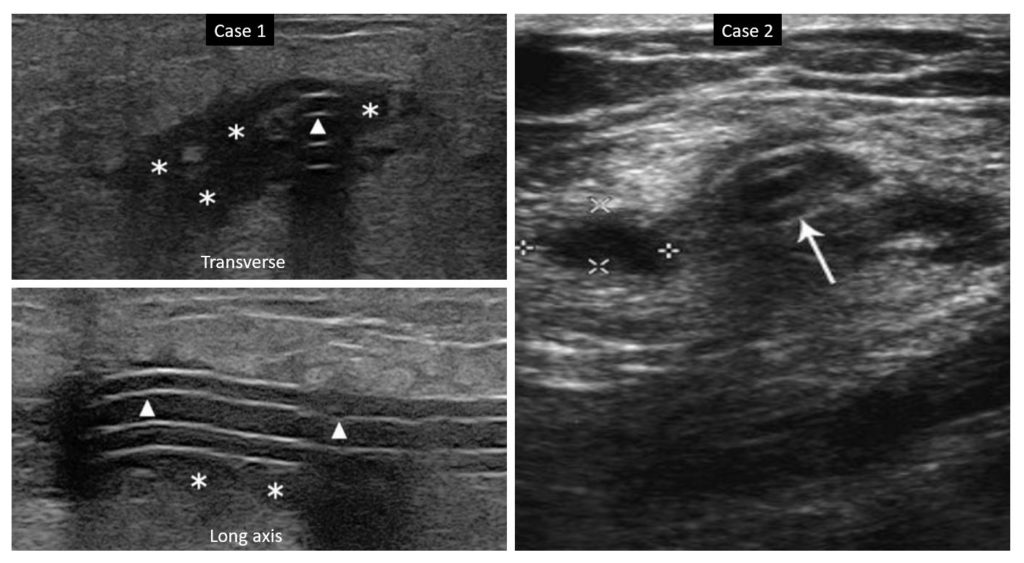
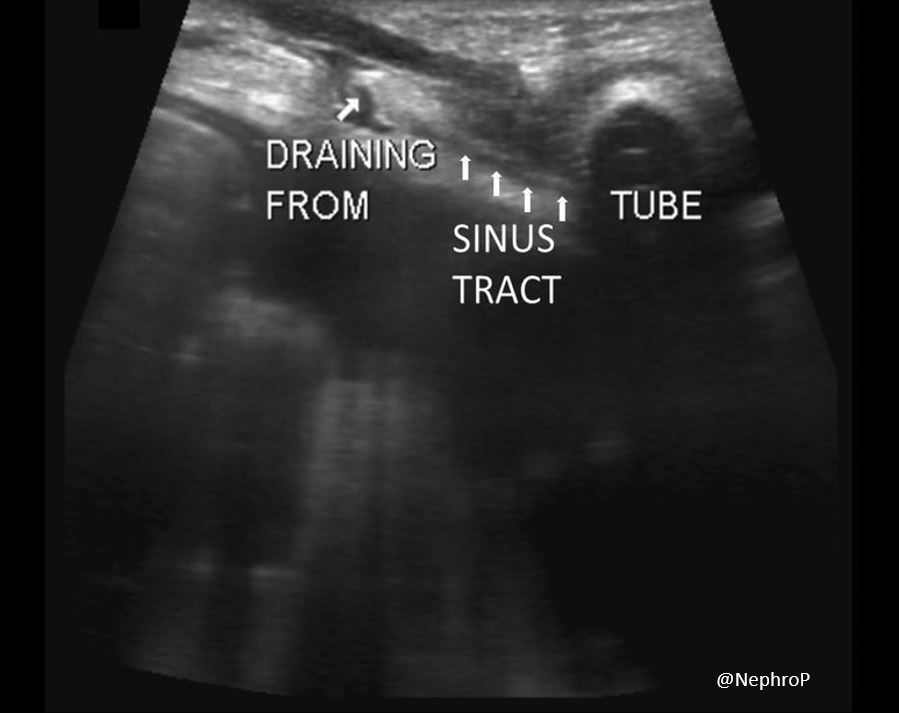
Figure 10 illustrates a case where the patient presented with peritonitis and serous drainage ~1 inch from the exit site. POCUS showed a sinus tract connecting the draining site and the inner segment of the catheter tunnel.
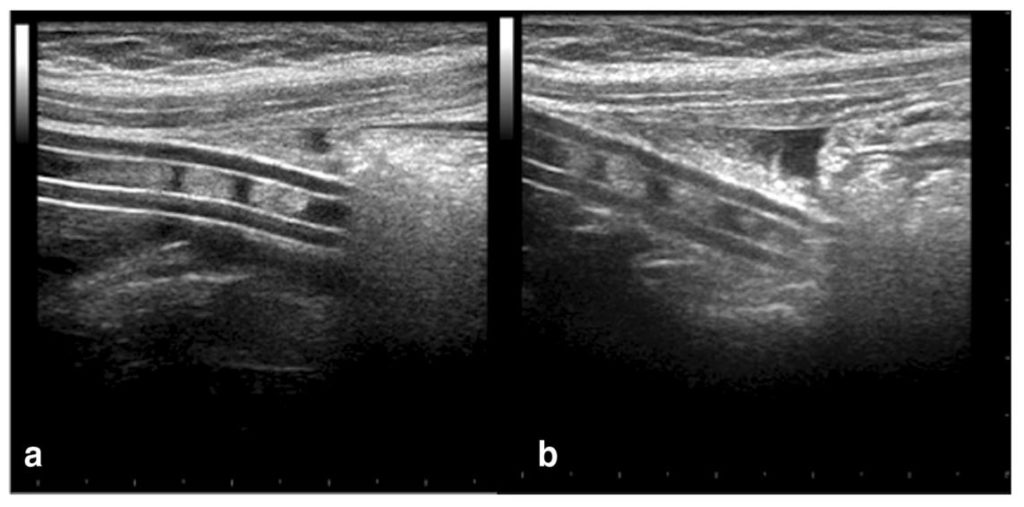
In kids due to their limited abdominal fat, the catheter tip may be located using POCUS and presence of debris within the catheter or presence of material at the tip of catheter can also be identified. Figure 11 shows the presence of echogenic material fragmented into the lumen (a) and around the distal tip (b) of the catheter in a child with PD catheter malfunction. It may be possible to see this in thin adults with limited abdominal fat.
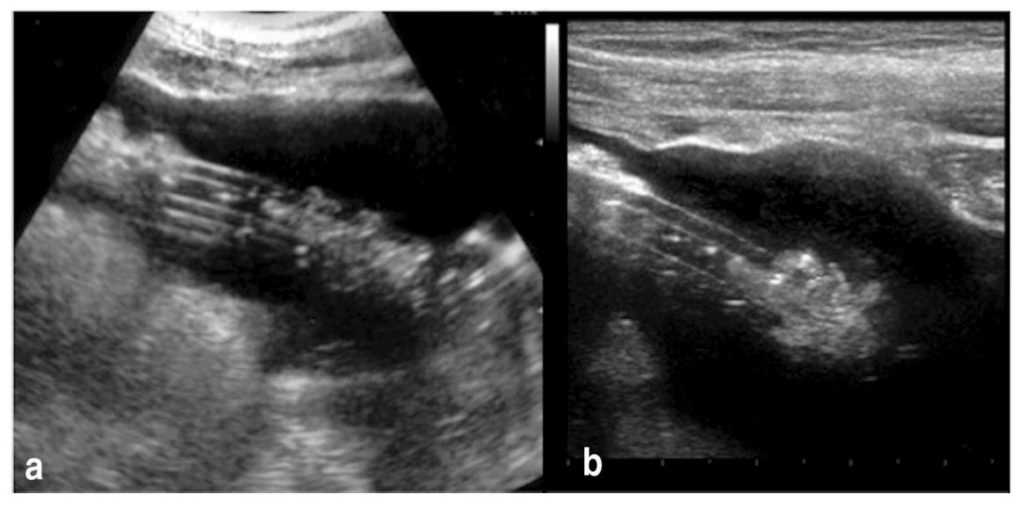
Here is another sonographic image [Figure 12] demonstrating amorphous material as homogeneous hyperechoic area in the lumen of the PD catheter (a) and around distal tip (b).
Tracing the catheter by ultrasound is not always a replacement for the use of CT scan or peritoneograms. If any leak or malposition is suspected, peritoneogram can be performed by interventional nephrology/radiology to address the cause.
Sayee Sundar Alagusundaramoorthy, MD
Interventional Nephrology Fellow
University of Wisconsin Hospital and Clinics



Hello. I think x Ray abdominal is important and can help for diagnostic.
I am looking for tunneled catheter because i know to make a tunneled catheter without ultrasound.