Casey Derella
PhD Candidate
Augusta University
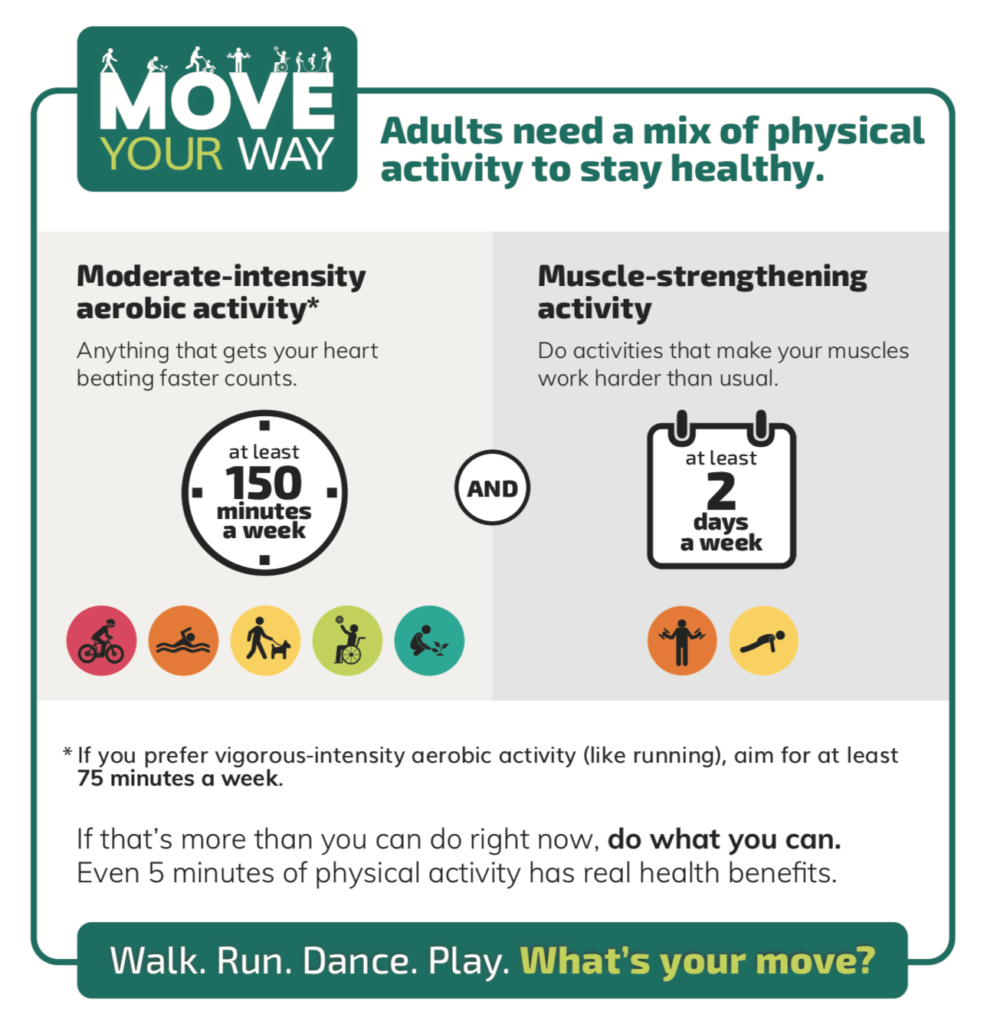
Exercise and physical activity of any kind provide a substantial number of health benefits. In fact, the 2018 Physical Activity Guidelines from the American College of Sports Medicine (ACSM) recommend that some exercise is better than none. However, 150 minutes of moderate-intensity exercise per week remains the ‘gold-standard’ for adults to gain substantial health benefits. Physical activity can make people feel, function, and sleep better, and reduce the risk of a large number of chronic diseases. The evidence about the health benefits gained from regular physical activity is well established, however, we continue to conduct research to understand what works to get people moving and to provide insight on how exercise can benefit various patient populations.
The 2018 ACSM Physical Activity Guidelines expanded on the physical activity recommendations for adults living with chronic conditions. These recommendations developed as we have gained a better understanding that certain modalities and intensity of exercise are not necessarily the best options for everyone. There are a number of chronic conditions and disabilities, but the ACSM Guidelines particularly focused on activity in adults living with osteoarthritis, type 2 diabetes, hypertension, adult cancer survivors, Parkinson’s disease, multiple sclerosis, spinal cord injury, and stroke. Based on current guidelines, those living with a chronic condition or disability, if able, should do:
- At least 150 to 300 minutes a week of moderate-intensity, or 75 to 150 minutes of vigorous-intensity aerobic physical activity.
- Muscle-strengthening activities of moderate or greater intensity that involve all major muscle groups on 2 or more days a week.
Research has demonstrated that the combination of aerobic and strength training can provide additional health benefits, particularly to those living with chronic conditions. Perhaps most important, the guidelines emphasize that if adults living with chronic conditions or disabilities are unable to meet the above recommendations, they should engage in regular physical activity to the best of their abilities and avoid inactivity. While the conditions included in the ACSM Physical Activity Guidelines are highly prevalent conditions in the United States, adults living with chronic kidney disease (CKD) were not specifically included in these suggestions. Exercise has many known benefits, and the current evidence supports the idea that regular physical activity in specific patient populations can have greater health benefits for these individuals.
It is estimated that 30 million adults in the United States have some stage of CKD, one of the most costly diseases in the world. Therapies to improve outcomes and slow disease progression remain inadequate. Physical dysfunction and muscle atrophy are often observed in patients with CKD and both contribute to a loss of independence and functional status- two important priorities to patients with CKD. More importantly, the progression of inactivity and muscle atrophy appear to increase with the worsening of CKD overtime. Given some of the limited physical function of patients with CKD, there is great potential that small amounts of exercise could have meaningful, positive impacts on their wellbeing. More importantly, could exercise help slow the progression of CKD?
In a review article by Drs. Johansen and Painter, they discuss the association between physical activity and kidney function, however this relationship remains controversial. A study from 2008 had patients with CKD (mean estimated glomerular filtration rate [eGFR] 29.9±17.0 mL/min/1.73 m2) complete a treadmill test (peak oxygen uptake), physical performance measures (sit to stand, gait speed, and 6-minute walk), and health status questionnaires. The authors did not observe a correlation between maximal oxygen consumption (VO2peak) and eGFR, but a positive correlation between maximal gait speed and eGFR was observed. In contrast to this study, Clyne et al observed a significant positive relationship between GFR and maximal exercise capacity after adjustment for age, sex, and hemoglobin concentration in men and women with CKD (GFR ranging from 3-32 mL/min/1.73 m2). In human studies, there appears to be an overall positive relationship between exercise and slowing CKD progression, with exercise improving various markers of kidney function decline. However, the disagreement between the results of these studies could be related to the heterogeneity of CKD, the modality and intensity of exercise used, the outcome measures, and poor study design (not controlling for sex, age, stage of disease, baseline values, etc). The heterogeneity of kidney disease in humans is a confounding factor we can’t control for, however, the use of animal models provides an opportunity to better understand how exercise can more directly impact CKD progression.
Avin et al is an example of a study that took advantage of utilizing an animal model to further investigate the impact of exercise in kidney disease. In this study, researchers utilized a rat model of progressive polycystic CKD (Cy/+IU on a Hans-Sprague Daley background) to investigate the hypothesis that voluntary wheel running would improve musculoskeletal health and slow kidney disease progression. This rodent model has a genetic mutation in Anks6, encoding for the protein SamCystin located at the base of cilia, and alters the nephronophthisis complex. Rats with this mutation spontaneously develop CKD with mineral-bone disorder that corresponds to stage 2-3 CKD in humans. In this study, researchers decided to model human access to exercise by providing a freely accessible activity wheel for the rodents to voluntarily utilize over the course of the study. At 25 weeks of age, male rats were given access to a voluntary running wheel or a standard cage condition (no wheel) for 10 weeks. Cage activity, grip strength, maximal aerobic capacity, and body composition were measured at both the start and end of the study. At the end of the 10 weeks, serum biochemistries (creatinine, phosphorus, parathyroid hormone), tissue weight, and bone micro-CT and mechanics were measured. The key findings from this study were:
- Male rats with kidney disease ran less than wild-type littermate rats.
- An inverse relationship with disease progression and physical activity was observed, meaning that as kidney disease progressed, the distance the rats ran decreased as well.
- Exercise had some benefit in rats with kidney disease.
- Overall statistical significant improvements in serum biochemistries in the rats with kidney disease that were given access to a wheel:
- creatinine: 1.26±0.9 vs 0.99±0.58 mg/dL
- phosphorus: 6.14±1.09 vs 5.17±1.31 mg/dL
- parathyroid hormone: 803±539 vs 521±198 pg/mL
- Overall statistical significant improvements in serum biochemistries in the rats with kidney disease that were given access to a wheel:
This is relevant to human patients with polycystic kidney disease that leads to kidney functional decline and confirms that kidney disease itself is associated with a progressive decline in physical activity, independent of age and comorbid conditions (both controlled for in the study). These findings are in line with those from human studies, and here suggest that even some voluntary exercise had a beneficial effect on disease progression in this model.
Using a different animal model of CKD (spontaneously hypertensive rats [SHR] with a ⅚ nephrectomy), Kohzuki et al assessed the effect of moderate chronic treadmill exercise on kidney function. This study also included antihypertensive therapy in a few of the groups, but for the purpose of this post, we are focusing on the exercise vs non-exercise groups only. Male mice were subjected to exercise training using a treadmill at 20 m/min, 0 grade incline, for 60 minutes, 5 days a week for 4 weeks (this intensity corresponds to 65% of VO2max). Blood pressure, body weight, 24 hour urine volume, urinary Na+, K+, and urinary protein were measured before and after exercise every week. Following the 4 weeks of training, animals were sacrificed to determine serum protein, albumin, glucose, urea nitrogen (BUN), creatinine, total cholesterol, and triglycerides. Focal glomerular sclerosis (IGS) was also determined with the kidney remnants. After 4 weeks of moderate exercise training, this study found that:
- Exercise has kidney-protective effects in this rodent model.
- Urinary protein excretion was significantly reduced in rodents in the exercise condition compared to non-exercise animals.
- Moderate exercise training significantly protected against increases in IGS.
Using two different models of kidney disease, Kohzuki et al and Avin et al provided support for exercise to help slow the progression of CKD. One observation from the Avin et al study that stuck out to me in particular, was that the animals with kidney disease and access to an activity wheel were more active than those with kidney disease and no wheel access, despite no incentive to be more active. While the non-exercise group did not have access to a wheel, and therefore, of course were less active, these findings suggest that simply providing access to physical activity could increase overall activity in patients with CKD. This observation is intriguing since more often than not, the primary reasons for low physical activity are access and time. Patients with CKD who receive dialysis treatments often do so 2-3 times a week and can therefore be limited in both extra personal time and access to safe and healthy exercise options. However, this study suggests that simply providing the access for patients could increase activity levels in these individuals. However, it is important to note that human behavior and motivation are extremely complex, and the human environment is not as easily controlled. Nonetheless, it is possible that incorporating opportunities for physical activity in treatment plans for patients with kidney disease could improve their health and care.
Current basic and clinical research present exciting observations that highlight the potential benefits of moderate intensity exercise among patients with kidney disease. Importantly, the activity levels described in the basic studies discussed here align with the 2018 ACSM Physical Activity Guidelines, that any activity is better than no activity. For patients that are limited in time and mobility, like patients with CKD, providing access and allowing people to dictate their own intensity level, may provide greater benefits than a strict regimen. While some basic and clinical studies have revealed potential benefits of exercise for patients with kidney disease, there is still a significant amount of research that needs to be done to better our understanding of how exercise specifically benefits patients with CKD.
Reviewed by: Elinor Mannon, Kelly Hyndman, PhD, Matthew Sparks, MD, FASN FAHA
If you enjoyed reading this post and are interested in learning more about exercise and how it relates to patient and kidney health, consider checking out these resources on RFN:
How would you improve dialysis care if you had unlimited resources?
Saturday Night Acute Kidney Injury
Urine Sediment of the Month: Colorless, Transparent Hyaline Casts