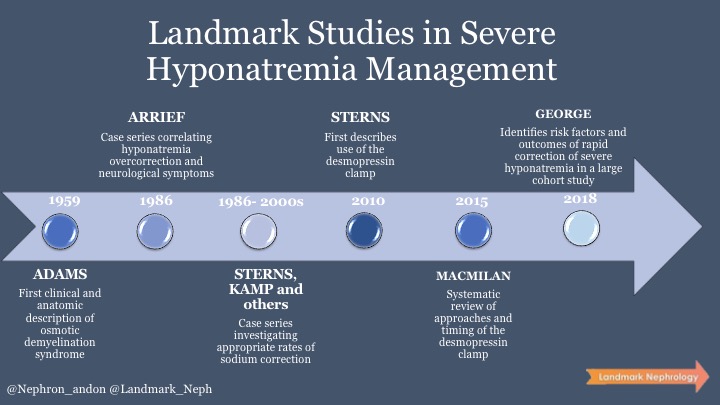
From the early physiology courses in Medical School, everyone learns to be wary of rapidly correcting serum sodium in the event of hyponatremia if its duration is chronic or unknown. But was this concern always present?
In the pathology literature, the anatomical and histological description of central pontine myelinolysis was first reported in 1969 in Boston involving four different cases with similar lesions. In this short case series, all patients had a background of alcohol use and malnutrition. They developed focal neurological symptoms including pseudobulbar palsy and quadriplegia, dying shortly thereafter. At that point in time, no link with hyponatremia had been definitely established yet as basic metabolic panels were not performed as frequently.
In the 1980s, there were a lot of discussion about the potential causative role of hyponatremia in the reported cases of neurological damage. Some believed that comorbidities were responsible while others identified the electrolyte itself as the culprit. In an attempt to disentangle the disease pathophysiology, Arieff described 15 different cases of women without comorbidities who developed acute hyponatremia after elective surgery. It was observed that about 48 hours after their interventions, these patients developed grand mal seizures in the context of an average sodium level of 108 mmol/L. During the course of these described cases, a broad array of differential diagnoses was considered and multiple different specialties were consulted including psychiatry. Two patients even underwent brain biopsies! The net result of these consults and investigations was that therapy for hyponatremia was delayed an average of 16 hours. The correction rate aim was about 0.5 mmol/L/h for most patients, which was considered a “slow correction” at the time. A specific pattern of neurological changes in response to overly rapid sodium correction emerged in this paper beginning with seizures, followed by transient improvement, followed by a lucid interval, and then finally a clear deterioration in their neurological status characterized by decreased alertness, increasing headache, nausea, and progressive obtundation. They found that all of these patients with worse outcomes had achieved sodium correction within 22 hours in comparison to the other patients, whose correction stage lasted 48 hours. Shockingly, 27% of the patients died, 13% had limb paralysis, and 60% were left in a persistent vegetative state.
The key unknown at this point was how quickly to correct sodium in order to avoid death and severe neurological impairment. In another landmark paper in the NEJM by Sterns, he again described the connection between rapid correction of serum sodium and neurological demise but reported from their own small case series and review of the existing literature that patients who had a correction rate below 12 mmmol/L/day did not suffer the phenomenon that they then described as ‘osmotic demyelination syndrome’. Another case series in 1993 argued that the rate of change be lowered to 10-12 mmol/L in 24 hours and 18 mmol/L in 48 hours. However, a clear caveat of all these recommendations is that they generally come from small case series as opposed to high-quality observational data or trials.
In the 2013, the concept of “clamping” was first proposed in which the use of desmopressin was suggested as a ‘clamp’ to avoid the dreaded overcorrection in hyponatremia. Sood et al first described the use of the desmopressin clamp in a quality improvement study in which 25 patients admitted to a community teaching hospital were treated for serum sodium level <120 mmol/L with concurrently administered desmopressin and hypertonic saline solution. No over- or under-correction was observed, and no adverse effects were reported associated with this treatment strategy. A systematic review in 2015 identified 17 observational studies with 80 patients in which the ‘desmopressin clamp’ was used. They describe several strategies in which it may be employed including 1. Proactive, where desmopressin is administered early based on initial serum sodium concentration; 2. Reactive, where desmopressin is administered based on changes in serum sodium concentration or urine output; and 3. Rescue, where desmopressin is administered after serum sodium correction targets are exceeded or when osmotic demyelination appears imminent. A proactive strategy of desmopressin administration with hypertonic saline appeared to be associated with lower incidence of exceeding serum sodium concentration correction targets, particularly in high risk patients.
To better understand who is considered high risk of rapid overcorrection of serum sodium (e.g. younger age, females, schizophrenia, lower Charlson comorbidity index, lower presentation serum sodium, and urine sodium <30 mEq/L) take a look at this recent retrospective cohort study of nearly 1500 patients serum sodium <120 mEq/L to seven hospitals in the Geisinger Health System. Eight (0.5%) patients had incident osmotic demyelination, of whom five (63%) had beer potomania, five (63%) had hypokalemia, and seven (88%) had sodium increase >8 mmol/L over a 24-hour period before magnetic resonance imaging.
Further controversial questions in symptomatic hyponatremia management include the bolus versus slow continuous infusion of hypertonic saline debate, which may have been just answered at ASN Kidney Week 2020 in favor of bolus doses.
Take a look at these other useful resources, review, and guidelines:
- An excellent, recent review from Richard Sterns
- Guidelines from the US and Europe
- NephMadness Hyponatremia Bracket 2018
- NephJC – ‘Does fluid restriction work for hyponatremia?’
Written by : Larissa Kruger @nephron_andon
Edited by: Jeffrey William @jhwilliamMD, Melanie Hoenig @melhoenig and Stewart Lecker @StewartLecker