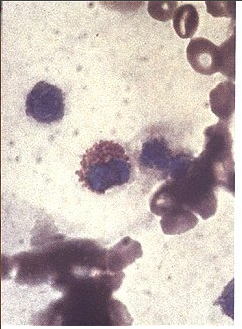
 Testing for the presence of urine eosinophils is often performed when the diagnosis of acute interstitial nephritis is suspected. The landmark paper touting the use of this test is a 1986 New England Journal of Medicine article by Nolan et al in which the use of the Hansel’s stain to identify urine eosinophils is first described. Prior to this, a Wright’s stain was used but the Hansel’s stain results in a bright orange staining of eosinophil granules that allows them to be much more easily differentiated from other white blood cells. In this paper, eosinophiluria was noted in 10 of 11 patients with AIN and in 0 of 30 patients with ATN, leading the investigators to suggest that the presence of eosinophils can be used to differentiate between these two common causes of AKI.
Testing for the presence of urine eosinophils is often performed when the diagnosis of acute interstitial nephritis is suspected. The landmark paper touting the use of this test is a 1986 New England Journal of Medicine article by Nolan et al in which the use of the Hansel’s stain to identify urine eosinophils is first described. Prior to this, a Wright’s stain was used but the Hansel’s stain results in a bright orange staining of eosinophil granules that allows them to be much more easily differentiated from other white blood cells. In this paper, eosinophiluria was noted in 10 of 11 patients with AIN and in 0 of 30 patients with ATN, leading the investigators to suggest that the presence of eosinophils can be used to differentiate between these two common causes of AKI.
Utility of Testing For Eosinophiluria
However, a more recent 2008 NEJM correspondence by Andrew Fletcher points out that subsequent studies looking at the utility of eosinophiluria to diagnose AIN are problematic. The author points out that at his institution, the sensitivity and positive predictive value of eosinophiluria for AIN were 25% and 3%, respectively. Furthermore, there is a wide variety of other diagnoses that can cause eosinophiluria, not just AIN. A brief differential diagnosis is as follows:
-acute interstitial nephritis
-renal atheroembolic disease
-bladder Schistosoma infection
-chronic pyelonephritis
-rapidly progressive glomerulonephritis
The Fletcher letter implies that based on the severe limitations of using the eosinophiluria to diagnose AIN that it not be used at all. I still use it, though based on these limitations it can probably only be used as an adjunct to make a diagnosis of AIN when trying to differentiate between AIN & ATN, a not uncommon scenario. Any other opinions out there as to how to best use this test?


